A Quantitative Approach to Vaccine Funding
By Coefficient Giving @ 2025-05-30T12:51 (+25)
This is a linkpost to https://www.openphilanthropy.org/research/a-quantitative-approach-to-vaccine-funding/
Introduction
At Open Philanthropy, we often use the Importance, Neglectedness, and Tractability framework when making decisions about how to prioritize spending across cause areas. In this post, we apply the framework to vaccine research and development (R&D) by comparing potential vaccine targets using metrics of importance and neglectedness.
Our main takeaway from this exercise: some diseases that kill many people receive very few resources for the development of cures and vaccines. In relative terms, R&D funding varies by 10 times or more across infectious diseases, often without good reason.[1] This disparity suggests that science funders could find unusually high-impact opportunities by targeting the most neglected diseases.
We use importance-neglectedness analysis like this as a starting point for more specific scientific landscapes and grant investigations focused on tractability. Taken together, these analyses have led us to believe that group A streptococcus (strep A) vaccines, syphilis vaccines, and hepatitis C vaccines are promising areas for philanthropic support of vaccine development. (There are other areas we believe are also high impact, but for reasons that have less to do with field-level neglectedness, and are more to do with importance and tractability.)
Past work on vaccine R&D
Since 2016, around 30% (or more than $150 million) of our grantmaking in scientific research and global health R&D has been related to vaccine R&D (inclusive of clinical trials).
We have made five or more grants for vaccine development in:
- Malaria
- Tuberculosis in adults and adolescents
- Strep A and rheumatic heart disease
- Syphilis
- Cross-cutting vaccine tools (computational models, animal models, new clinical protocols, new adjuvants, etc.)
We have also made grants in other areas of vaccine research when an opportunity seemed particularly strong. Sample areas include influenza, cholera, hepatitis E, schistosomiasis, and cancers (prophylactic).
Data sources and methodology
To compare importance and neglectedness, we started by listing 84 prominent infectious diseases and etiologies that prophylactic vaccines could target by combining the list of communicable causes of death or injury from the Global Burden of Disease (GBD) study,[2] the etiologies for which GBD provides estimates,[3] CEPI’s priority pathogens list, and a few other diseases and etiologies we felt were relevant.
To generate initial estimates of the “importance” for each of these 84 targets, we used the GBD’s forecasts for how many Years of Life Lost and Years Lived with Disability are expected from each. To generate initial estimates of “neglectedness”, we used (1) funding data for poverty-related diseases from the annual G-FINDER survey[4] and (2) information on the number of vaccine products that are currently available to the public, mainly from Saloni Dattani’s vaccine timeline dataset, supplemented by information from the U.S. FDA and the WHO. This list is unlikely to capture every vaccine, but we think it’s a relatively complete starting set.[5]
Importance and neglectedness metrics
By connecting these data sources, we can compare different diseases/etiologies across useful indicators of importance and neglectedness. For example, the table below shows the top 25 targets in terms of future disease burden. We specifically look at the estimated burden for the year 2050, since R&D investments today only pay off decades into the future[6] (making future burden a better way to assess the potential health impact of grants today).
After we filter by future burden, we look at a neglectedness metric. In particular, we compare the DALY burden to R&D funding according to G-FINDER[7] to get a ratio of dollars spent relative to the size of the problem. A disease that gets less R&D funding per projected DALY is more neglected, and may be more deserving of new funding (though in practice, we haven’t found this to be a perfect rule; we discuss some exceptions below).
Note: G-FINDER only measures a subset of total funding for each disease/etiology. See more details here, point #4.
Finally, we look at which shortlisted diseases and etiologies do not yet have a vaccine, to get a perspective on what new vaccine R&D could target. While this is a limited perspective — as we explain below (point #7), some diseases have imperfect vaccines in need of improvement — it can still provide useful context.
Table: Importance and neglectedness metrics of potential high-burden vaccine targets*
| Target | DALY forecast (2050, rounded) | R&D funding* per year (2019 to 2023 rounded average) | R&D$* per year/2050 DALYs | # of vaccines widely available (lower bound)* |
|---|---|---|---|---|
| Malaria | 33,500,000 | $703,000,000 | $21.0 | 2 |
| Tuberculosis | 24,800,000 | $795,000,000 | $32.0 | 1 |
| Hepatitis B | 23,000,000 | $21,000,000 | $0.9 | 3 |
| Hepatitis C | 21,800,000 | $18,000,000 | $0.8 | 0 |
| HIV/AIDS | 18,400,000 | $1,541,000,000 | $83.7 | 0 |
| Streptococcus pneumoniae | 17,800,000 | $48,000,000 | $2.7 | 6 |
| Group A streptococcus | 17,400,000 | $14,000,000 | $1.2 | 0 |
| Rotavirus | 10,600,000 | $32,000,000 | $3.0 | 4 |
| Staphylococcus aureus | 8,700,000 | 0 | ||
| Influenza | 8,000,000 | 11 | ||
| Pertussis | 7,800,000 | 5 | ||
| Shigella | 7,100,000 | $51,000,000 | $7.3 | 0 |
| Klebsiella pneumoniae | 6,300,000 | 0 | ||
| Adenovirus | 6,200,000 | $3.7 | 0 | |
| Cryptosporidium | 5,600,000 | $22,000,000 | $3.9 | 0 |
| Respiratory syncytial virus | 4,800,000 | 2 | ||
| Syphilis | 4,300,000 | $9,000,000 | $2.1 | 0 |
| Invasive Non-typhoidal Salmonella (iNTS) | 4,200,000 | $10,000,000 | $2.5 | 0 |
| Norovirus | 4,100,000 | $3.7 | 0 | |
| Enterotoxigenic E. coli | 4,000,000 | $9,000,000 | $2.3 | 0 |
| E. coli causing Meningitis/LRI | 3,500,000 | 0 | ||
| Enteropathogenic E. coli | 3,400,000 | $3.7 | 0 | |
| Typhoid fever | 3,400,000 | 2 | ||
| Cholera | 3,100,000 | $39,000,000 | $12.6 | 2 |
| Pseudomonas aeruginosa | 2,900,000 | 0 |
*See footnotes 4 and 6. Also, note that we didn’t count vaccines that were available only in very few countries, and that likely need more studies to become widely available (this was the case for Shigella and Hepatitis E). Similarly, we didn’t count the Adenovirus vaccine, since it’s only available for United States military personnel.
We make rough extrapolations where data was lacking. Figures in the table above that rely on these extrapolations are colored grey and in italics.
For example, for simplicity we assume that diseases and etiologies without GBD estimates will decline at the same rate as the average decline projected for diseases whose future impact GBD has estimated. When G-FINDER and GBD categories don’t match well, we use proxies to calculate the ratio of R&D funding to DALY burden (e.g., inputting the R&D$/DALY of diarrheal diseases as a whole for each specific diarrheal etiology). More details are available in the spreadsheet.
Takeaways
The analysis above provides a shortlist of potential vaccine R&D areas that may be worth further investigation. Here is a closer look at the top seven targets in terms of burden, each projected to account for more than 15 million DALYs in 2050:
Chart: DALY forecast and R&D funding of the most burdensome diseases/etiologies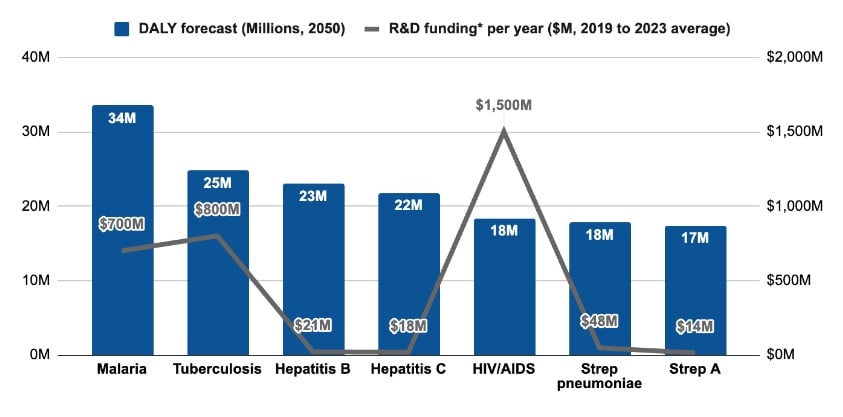
(Same units as previous chart)
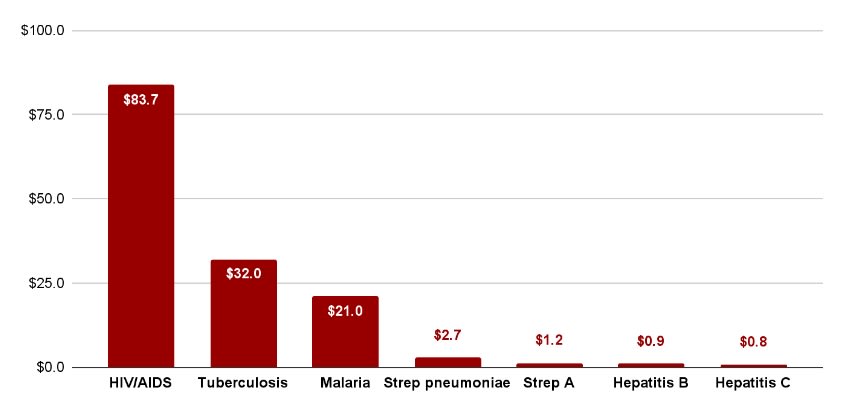
Note for both charts: G-FINDER only measures a subset of total funding for each disease/etiology. More details here, point #4. Figures were rounded.
These figures give us prompts for further investigation. For example:
- Malaria and tuberculosis (TB) are projected to have the highest burden in 2050, even though they receive more resources per DALY than many others on the list, and they already have 1-2 vaccines available. Why do they still have such a high projected burden?
- Short answer: the existing vaccines available for malaria and TB help to reduce cases and deaths, but need major improvements. Today’s malaria vaccines require four shots, and their efficacy wanes over a few years. The one available TB vaccine, BCG, works well in children but doesn’t provide reliable protection in adults. New vaccines are needed for both diseases, and that’s why we are investing in vaccine R&D for them (examples: malaria, TB).
- Hepatitis C, hepatitis B, and streptococcus pneumoniae affect lots of people in high-income countries. Why do they have such little R&D investment, given that those markets are more lucrative for product developers?
- Short answer: The G-FINDER data we use excludes funding aimed primarily at markets in high-income countries (HICs). For example, it only counts hepatitis B research if it’s explicitly targeted at low- and middle-income country (LMIC) needs — like studying HBV mutations in LMIC populations. This exclusion makes sense for some purposes, but it also means total R&D spending on these diseases is likely much higher than what appears in this analysis. More on G-FINDER data below (point #4).
- Hepatitis B already has several vaccines. Why is it still expected to cause such a high burden in 2050?
- Short answer: hundreds of millions of people worldwide are already chronically infected with hepatitis B, often adults who were never vaccinated in childhood. Over time, many of them will develop liver complications. Meanwhile, many LMICs struggle to deliver the critical birth-dose vaccine within 24 hours of birth (coverage is just 17% in Africa), leaving newborns vulnerable to mother-to-child transmission. Given both of these factors, developing a cure for Hepatitis B could be unusually impactful. Innovations in vaccine delivery (e.g., microneedle arrays) may also help drive down the burden. We don’t see a major need for entirely new vaccines; the existing ones are very effective.
- HIV/AIDS receives the most resources out of the diseases/etiologies analyzed. Why don’t we have a vaccine yet?
- Short answer: there are several scientific hurdles associated with creating an HIV/AIDS vaccine. HIV mutates rapidly, integrates into host DNA, and evades the immune system in ways that make vaccine development difficult. Other approaches, such as long-acting antiretroviral therapy, may be more tractable to reduce disease burden.
- Strep A and hepatitis C have among the lowest R&D$ per DALY, and neither has a vaccine. Why don’t they receive more funding already? Is it too hard to develop vaccines against them?
- Short answer: We think developing vaccines against strep A and hepatitis C is feasible. These targets are not trivial, but we don’t believe they present the same degree of challenge as developing an HIV/AIDS vaccine (we are more confident about that with strep A than hep C). Vaccine development for both seems promising and could help reduce global burden significantly, especially alongside expanded access to treatment. The potential for new vaccines has led us to make grants in vaccine R&D for both strep A and hepatitis C.
Limitations
While this was a valuable exercise, we do not take these R&D$/DALY numbers “literally” without further context. That is for a few reasons:
- Burden projections are uncertain. The GBD study has one of the best collections we’ve seen of estimates for future disease burdens. Still, any estimate of this kind is subject to numerous uncertainties, often resulting in wide confidence intervals.[8] Before making grants in a new disease area, we try to understand the epidemiological assumptions underlying GBD’s burden estimates in more depth. For example, TB burden is likely to follow a more “predictable” trajectory than malaria, since TB has a relatively long latent phase and slower human-to-human transmission, while malaria burden responds to more volatile factors such as mosquito population (which is sensitive to changes in climate) and can reemerge explosively in countries where it had been nearly eradicated before.
- Most pathogens with future pandemic potential are excluded. If we had carried out this same exercise in 1980, HIV/AIDS would not have appeared in our table (the first AIDS cases were reported in 1981), despite that condition being the top global infectious disease killer 25 years later. The table above is useful for existing endemic diseases, but less useful for diseases that could spread in the future. Building mostly off of CEPI’s priority pathogens list, here are some viruses that could trigger public health emergencies:
- Chikungunya
- Ebola
- Influenza
- Lassa Fever
- MERS
- Mpox
- Nipah and Hendra
- Rift Valley Fever
- Zika
- Not all R&D funding is equally useful. Often, scientific fields are lacking new ideas or new talent, rather than “just” funding. Our experience in Alzheimer’s research, for example, is that some funding is as good as wasted, whereas other funding can be quite impactful. Which is which? That’s often hard to predict ahead of time, and different funders can reasonably disagree about which efforts are promising. Nevertheless, looking at total funding levels for each disease is a useful starting point for neglectedness analysis.
- The funding data we used excludes some R&D spending. G-FINDER estimates don’t include all R&D funding, as they follow 3 main inclusion criteria: the disease disproportionately affects LMICs, a new product is needed in that product category, and there is “market failure” (i.e. there is an insufficient commercial market to attract R&D from private industry). This can lead to lower investment figures than one would expect. For example, R&D spending on microbicides against HIV/AIDS that can be sold in high-income country (HIC) markets is excluded from G-FINDER’s scope (p. 24), and the hepatitis C funding number is lower than we believe is reasonable for our purposes.[9] Also, we excluded funding to cross-cutting applications (e.g. platform technologies) and funds categorized for more than one disease/etiology.
- Disease/etiology groupings are inconsistent between sources. For example, disease/etiology categories from GBD do not always match how G-FINDER defines a disease or disease group. We matched GBD and G-FINDER terminology as best we could for practical purposes, but this has likely resulted in some over/underestimates of funding.
- Some categories already have effective products. If a disease category already has effective products, there may be less need for new R&D, so it may look “artificially” neglected. For example, syphilis can be detected (imperfectly) with a rapid test that costs less than a dollar, and treated with benzathine penicillin G, which also costs less than $1 per dose and has shown little detected resistance. So, while a syphilis vaccine would still be valuable,[10] syphilis gets relatively little funding as a whole because funders have less reason to invest in developing new treatments.
- The number of vaccines doesn’t tell the whole story. Even if a disease has zero vaccines, that doesn’t necessarily mean that developing a vaccine would be the best way to reduce its burden through R&D; sometimes, investments in clean water and reducing malnutrition are better approaches. And on the other hand, developing new vaccines may sometimes be the best way to reduce health burden for diseases that already have vaccines (e.g. because existing vaccines aren’t sufficiently durable or effective).
- Not all harms are captured by DALYs. For example, helminths don’t appear in the table above listing the top 25 vaccine targets in terms of health burden, but the main reason GiveWell recommends deworming interventions is their impact on educational outcomes rather than on mortality or morbidity.
- We made some rough extrapolations. As mentioned previously, we made some rough extrapolations to fill data gaps. These extrapolations are better than nothing, but can make our work look more objective and certain than is warranted given the weakness of the primary data.
- Products don’t exist in a void. For a new health technology to be useful, people who could benefit from it must be able to access it, as well as want to use it. Health burden numbers alone can’t predict that well. For example, delivering vaccines to adults tends to be more complicated than delivering vaccines to children in most countries;[11] stigma related to sexually transmitted infections may make a syphilis vaccine less popular than a malaria vaccine; R&D work would be less impactful across the board if donor countries reduce their support for Gavi to distribute vaccines; and so on.
Conclusion
Even with the above limitations in mind, this exercise reaffirmed a striking pattern: some diseases get much less R&D funding (relative to others) than their future health burden suggests would be beneficial. That gives us a useful place to start when figuring out which disease areas might be productive to investigate for grantmaking. Alongside recommendations from people in the global health community,[12] analysis of this form has led us to investigate — and make — grants related to strep A, syphilis, and hepatitis C vaccine development. Similar analysis led to grantmaking in other neglected areas outside of vaccines such as development of cures for hepatitis B, technical assistance for sickle cell disease screening and treatment, and development of antivenoms for snakebites.
Appendix: All data + analysis
Here is the spreadsheet with our data analysis (we suggest you read the limitations section before opening that link). The main tab lists potential diseases and etiologies new vaccines could target, then characterizes each of these “targets” by how many vaccines exist for them, their estimated burden, their R&D funding, etc. The summary tab shows key analyses, including the one that led to the table above. Other tabs serve as input for the main tab.
We appreciate any feedback on the spreadsheet or this post; please share it with rafael.dib@openphilanthropy.org.
- ^
This finding mirrors the 10/90 gap discussed over the previous generation of global health research. Our analysis here is more specific to particular diseases, rather than the disparity between higher-income and lower-income countries per se.
- ^
Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Study 2021 (GBD 2021). Seattle, WA: IHME, University of Washington, 2024. https://www.healthdata.org/research-analysis/gbd-data. First accessed on Sep 17, 2024.
- ^
Etiology is basically equivalent to pathogen in this context. We kept etiology as it’s the language used by GBD. Note that this does not include all communicable diseases and etiologies in GBD. COVID-19 was excluded because it’s hard to compare to other diseases, given its sudden peak and subsequent declines. Encephalitis wasn’t included as a whole because it seemed more useful to look at particular types of encephalitis. Similarly, we didn’t include meningitis or otitis media as diseases, but we did include most of their etiologies. Guinea worm disease wasn’t included because GBD estimated it only had ~1 DALY in 2021. “Chlamydial infection” disease from GBD was excluded because we already are looking at chlamydial spp. “Fungus”, “polymicrobial”, “other bacterial pathogen”, “viral etiologies of meningitis”, and other GBD etiologies of lower respiratory infections and meningitis were excluded because they are too generic for this exercise. “Non-typhoidal Salmonella” GBD etiology was excluded because it could have an overlap with iNTS, which was included.
- ^
Impact Global Health, G-FINDER data portal 2024, https://gfinderdata.impactglobalhealth.org. Accessed on Nov 25, 2024.
- ^
We looked at this information in November 2024 and relied heavily on Saloni Dattani’s dataset, which “shows when each vaccine was introduced for humans, for the first time. […] The dataset also shows new versions of some vaccines and when they were made available. This hopefully covers most of them but is likely incomplete, and it was harder to track down the exact years for several historical ones.” Note that vaccines are not included if they were withdrawn or never made widely available.
- ^
A good rule of thumb is that it takes ~20 years to go from science to technology. Once a new vaccine is approved, it also takes a number of years to be integrated into health systems to provide maximal benefit.
- ^
Note that G-FINDER includes only a subset of total funding; see more details here, point #4.
- ^
For example, while the reference estimate of the malaria burden in 2040 is ~36 million DALYs, its 95% confidence interval ranges from ~12 million to ~84 million DALYs.
- ^
The pharmaceutical industry has made substantial investments into drug development for hepatitis C, but many of those investments are excluded from G-FINDER because they target high-income country markets. However, some of those investments are starting to benefit LMICs too, as drugs developed in high income countries become available in lower income countries.
- ^
For example, vaccinating pregnant women is expected to not only provide personal protection but to reduce the risk of fetal mortality or birth defects caused by the syphilis bacterium, which can cross the placental barrier.
- ^
Immunization efforts are often integrated with maternal and child health services. In addition, adults don’t have as many routine contact points with health systems.
- ^
A tip from George Rugarabamu for rheumatic fever, and from Damian Walker for syphilis, to name a couple. Thank you!
SummaryBot @ 2025-06-03T16:18 (+1)
Executive summary: Open Philanthropy presents a quantitative framework for identifying promising vaccine R&D targets by analyzing disease burden and funding gaps, concluding that diseases like group A streptococcus, syphilis, and hepatitis C are particularly neglected relative to their projected future impact and merit greater philanthropic investment.
Key points:
- Framework and main finding: Applying an importance-neglectedness framework to 84 infectious diseases reveals significant disparities—some high-burden diseases receive up to 10x less R&D funding than others, suggesting overlooked opportunities for impact.
- Top neglected targets: Group A streptococcus, hepatitis C, and syphilis have among the lowest R&D funding per projected DALY in 2050 and no widely available vaccines, making them compelling candidates for philanthropic support.
- Methodology and limitations: Estimates are based on GBD projections, G-FINDER funding data, and vaccine availability, with acknowledged gaps (e.g. data exclusions, inconsistent disease groupings, and uncertainty in burden forecasts).
- Insights into specific diseases: Some high-burden diseases like malaria and TB already receive substantial funding but still lack effective vaccines; others, like hepatitis B, appear underfunded due to data exclusions (e.g. high-income country focus).
- Grantmaking implications: This analysis has informed Open Phil's vaccine grant portfolio and led to investments in other neglected areas such as hepatitis B cures, syphilis testing, and antivenom development.
- Broader cautions: The authors emphasize that quantitative metrics alone are insufficient; tractability, implementation context, and expert judgment are essential for effective prioritization.
This comment was auto-generated by the EA Forum Team. Feel free to point out issues with this summary by replying to the comment, and contact us if you have feedback.