[Cause Exploration Prizes] Increasing research funding into COPD
By Coefficient Giving @ 2022-08-29T10:58 (+11)
This anonymous essay was submitted to Open Philanthropy's Cause Exploration Prizes contest and published with the author's permission.
If you're seeing this in summer 2022, we'll be posting many submissions in a short period. If you want to stop seeing them so often, apply a filter for the appropriate tag!
Summary
- Chronic obstructive pulmonary disease (COPD) is a heterogeneous condition that causes breathing difficulties. It is the third leading cause of death worldwide and contributes to a significant proportion of disease burden globally.
- Despite its outsized impact on global health, funding for research into the biology and potential treatments of COPD has been lackluster. Depending on the comparison used, COPD research receives about 16 times less funding than breast cancer when adjusted for deaths caused by each condition.
- Increasing research funding into COPD may provide great future health and economic gains. Whether this impact passes Open Philanthropies’ 1000x bar is unclear and hard to determine based on insufficient means of measuring research impact and the long lag-time between research and clinical outcomes.
Note: This essay is the result of a shallow investigation into COPD and the disparities in biomedical research funding. While I work in immunology research, I am not familiar with the COPD field and this report is purely based on the desk research I have performed in the past few weeks. I personally believe this is a deserving area for more funding but there are a number of open questions I was not able to answer during my research, most importantly, whether research funding may clear Open Philanthropy’s bar of 1000x social return on investment.
How big of a problem is COPD?
Chronic obstructive pulmonary disease (COPD) is a condition that causes breathing difficulties and presents with heterogeneous clinical phenotypes, including emphysema and chronic bronchitis. COPD is the third leading cause of death worldwide and the sixth biggest contributor to disability-adjusted life years (DALYs) among all causes in 2019, causing 74.43 million DALYs and 3.28 million deaths.[1] In the UK alone, about 115,000 new cases are diagnosed every year.[2]
Common risk factors for the development of COPD include smoking, air pollution (both ambient and household), elevated ozone levels, ambient particulate matter, occupational particle exposure, and non-optimal temperatures. While the impact of smoking and household air pollution on the global COPD disease burden have decreased over the last three decades, they remain the leading risk factors together with exposure to ambient particulate matter pollution and occupational particle exposure. Notably, the contribution of ambient particulate matter pollution to disease burden is growing in low-income countries (LICs), as well as lower middle income countries (LMICs). Together with population growth and aging, as well as increasing impact of elevated ozone levels and high temperatures, COPD is likely to remain a major global issue, even if public health measures targeting tobacco will be successful.[3]
Besides the considerable health impacts of the disease, COPD also has economic consequences, both through direct costs associated with the treatment of COPD patients, as well as indirect costs (e.g. through lost productivity). There are a number of studies estimating the direct costs of COPD, most of which have been conducted in high income countries (HICs); significantly fewer studies consider indirect costs, but they are believed to be several times greater than direct costs in many countries. A US-based study has estimated direct costs of COPD to be $32 billion in 2010, with indirect costs adding an additional $20.4 billion.[4]
What are the currently available interventions that can address this problem?
COPD is a heterogenous disease, but generally patients have trouble breathing due to inflammatory processes within their lungs. During disease progression, there is a remodeling of the airways that further exacerbates breathing problems and is thought to be irreversible. The exact mechanisms underlying the disease are still unknown, but researchers have shown the importance of different parts of the immune system, including neutrophils, macrophages and a number of signaling molecules.
Currently, treatment of COPD is only targeting symptomatic relief and prevention of exacerbations. This is mainly achieved through the use of bronchodilators (short or long acting), which are recommended as first-line treatment. Bronchodilators relax smooth airway musculature which opens airways and makes breathing easier. Two different classes of bronchodilators are used in COPD. Usually patients only receive one bronchodilator, but if they remain symptomatic, combination therapies may be recommended. In addition to bronchodilators, treatment often includes inhaled corticosteroids for the management of inflammation.[5]
However, there is no disease-modifying treatment available at this point. Much work has been done to address COPD’s underlying inflammatory and remodeling processes, but so far very little of this has been translated into clinical practice.
What are possible research interventions?
There are many open questions concerning COPD and its underlying biology and treatment. In order to address the existing knowledge gaps, further development of research infrastructure may be warranted. This includes the identification of better and more reliable models, as well as increased access to patient material. Better models are needed as most animal models seem to be ill-fitted for respiratory disease research. Commonly used rodent models have distinct differences to humans regarding their airways, as well as immune system. Preclinical research may make use of models of human origin, such as organ-on-chip models. While current versions have a number of limitations, increased development in this field holds promise for disease modelling in the future.[6] Several lines of research require access to patient material. Cancer biology has profited significantly from the establishment of biobanks and COPD research may benefit from similar initiatives to learn more about the underlying biology of the condition.
Modern medicine increasingly moves away from “one-fits-all” approaches towards personalized treatments. Precision medicine is based on increasing understanding of the heterogeneity of diseases and their underlying biology, as well as associated biomarkers. COPD as a very heterogeneous disease has long been appreciated from a clinical perspective with different clinical phenotypes characterized.[7] However, more work is needed from a molecular characterization of patients[8], allowing for proper patient stratification for future clinical development. Inflammatory processes may be based on different pathways in different patients; most patients show neutrophil-driven inflammation, whereas others show increased infiltration of eosinophils.[9] Differences in underlying biology will require different therapeutic approaches. This has been shown in, for example, the treatment of cancer, where biomarker discovery has been successfully translated into personalized medicine, with targeted therapeutics being used dependent on biomarker status of patients. COPD may similarly benefit from a more personalized approach[10][11], which can only be implemented once we understand more about biomarkers and patient heterogeneity in COPD.
Another important topic in COPD management (but also other chronic lung conditions), is the development of steroid resistance, which is common in COPD. The prevailing view is that oxidative stress in the lung microenvironment of COPD patients seem to deactivate histone deacetylase 2, an enzyme necessary for the anti-inflammatory effects of steroids. Some drugs that target this pathway of steroid resistance are already in development for the treatment of COPD, but more work is still required. Examples include: theophylline (a PI3K inhibitor), the antidepressant nortriptyline, and macrolide antibiotics (the latter two both increase histone deacetylase-2 activity).[12][13] Treatments that target steroid resistance in COPD are not being tested adequately, given their potential impact on disease burden globally and the repurposing of existing and already approved drugs in this area may accelerate progress.[14]
Recently, considerable efforts have been made to identify new therapeutic approaches for COPD. In broad terms, treatments may target inflammation, tissue remodeling, oxidative stress, or a combination of these processes. Previous trials that evaluated the blockade of specific inflammatory cytokine pathways have been unsuccessful, likely owing to the heterogeneity of patients, as well as redundancies in inflammatory pathways. Testing these approaches in well-defined subpopulations may harbor more promise.[15] Other targeted approaches for reducing inflammation may be cell-specific, such as reducing the recruitment of neutrophils into the lung tissue, or utilizing the body’s own regulatory pathways, such as by adoptively transferring regulatory T-cells into COPD patients.[16] The delivery of these drugs is also an important topic. The immune system plays an important role in the body, and even though treatments may try to reduce immune activity in COPD, this has to be targeted to the site of inflammation to avoid the grave side-effects of systemic immune suppression. Inhalation is a straightforward method to bring medication into the lungs while avoiding systemic exposure, but drug discovery in this field is far behind.[17]
Other interesting areas of research include the relationship between the lung microbiome and COPD progression,[18] the differences between smoking-induced and air pollution-induced COPD, and the contribution of autoinflammatory processes to the progression of COPD.
The neglectedness of COPD research
As described above, COPD is a major contributor to disease burden worldwide and, importantly, has a high prevalence in both developed and developing countries. An analysis of research funding by 11 of the largest funders worldwide showed that in 2019 COPD research received $83.68 million in funding.[19][20] If we compare this to global disease burden of 74.43 million DALYs and 3.28 million deaths, we find that research funding amounts to $1.1 ($25.5) per DALY (death). This is contrasted by research funding in other common diseases, with research expenditure per DALY (death) to $14 ($412.6) for breast cancer, $17.8 ($620.3) for leukemia, $5.1 ($114.4) for colorectal cancer, $49.5 ($2730.9) for HIV/AIDS, $73.8 ($1149.7) for Alzheimer’s disease, $9.2 ($365.5) for tuberculosis, and $8.7 ($631.5) malaria (see Fig. 1). Notably, the same levels of disproportionate funding can be seen across countries and funding agencies, such as in the US, UK, and China.[21]
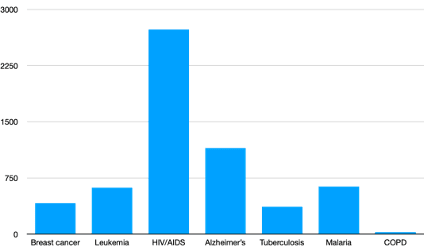
***Fig. 1 Research funding for different diseases adjusted for number of deaths caused by disease. *Data for research funding was taken from the WHO’s World RePORT which summarizes disease specific research funding for 11 of the largest funders worldwide. Data on deaths was sourced from the Global Burden of Disease 2019 dataset.
Another hallmark of the chronic underfunding of COPD research is the lack of clinical development. As of 2017, the NIH reported 7,857 ongoing clinical trials for breast cancer, and 5,360 trials for leukemia, whereas only 2,997 trials were targeting COPD. This highlights the lack of advancement of basic and clinical research into the disease, as these lay the foundation for clinical development of new drugs.[22]
COPD research is underfunded for a number of reasons. Due to its link to smoking, COPD is often seen as a self-induced disease, which makes people reluctant to donate to nonprofits supporting COPD research. This explains reduced funds available from private foundations. In 2017, the US Breast Cancer Research Foundation and the Leukemia & Lymphoma Society were awarded $59.5 million and $40.3 million for research projects, respectively.[23] The COPD Foundation’s total research budget for the year 2021 amounted to $5.3 million.[24]
At the same time, COPD disproportionally affects poor segments of the populations, with risk factors such as tobacco use, air pollution, poor diet, poor housing, and occupational exposure closely linked to poverty.[25] In the UK for example, the poorest 20% of the country reportedly make up 85% of those living in areas with the highest levels of air pollution.[26] Poor patients also have fewer resources at their hands to lobby for increased research expenditure. In fact, COPD does not have a strong social movement around it. Patient activism is an important part of policy making process, with lobbying helping to attract funding towards certain diseases.[27]
Another reason for the lack of funding may be reduced enthusiasm around the COPD research field. Research findings that highlight promising pathways for treatment can attract more funding towards a specific disease. Examples of this are increased allocation of funding towards Alzheimer’s research in the wake of the amyloid hypothesis (as flawed as this may have been), as well as the development of immunotherapies in cancer after the discovery of immune checkpoints. However, research into COPD has not had many recent high-profile successes, which not only affects funding agencies but the research community as well. Research areas are much more likely to attract talented researchers when there is enthusiasm around a field. Furthermore, researchers are dependent on the availability of samples, drugs, and reagents. Past underfunding hampers the development of a research ecosystem around COPD, with much of the required infrastructure missing. Scientists are reluctant to move from well-established and well-funded fields into riskier areas and funding panels are more likely to consist of researchers from more established research areas, further reinforcing the status quo of funding inequalities.[28]
Overall, it is clear that COPD research is neglected in comparison to the impact of the disease worldwide. There are a number of reasons for this, including public perception, a lack of lobbying, and reduced enthusiasm around the area. Many of these reasons are part of a vicious cycle in which underfunding of research hampers the progress within a field and the development of functioning ecosystems, which in turn further discourages funding towards a certain disease.
Who else is working on this already?
Biomedical research is usually funded by a mixture of philanthropic, governmental, and corporate funds. As mentioned above, a number of the largest funders together allocated $83.68 million in funding to COPD research in 2019. Only 5 out of 11 organizations contributed to the disease, with the largest funder being the NIH, contributing $78.79 million to COPD research, followed by Canada’s CIHR with $2.05 million, the UK’s Medical Research Council (MRC) with $1.55 million, Sweden’s SRC with $0.75 million, and the Wellcome Trust with $0.54 million.[29] Other governmental funders include the Natural Science Foundation of China, which allocated between $1.9 million[30] and $4.7 million[31] towards COPD research in 2012. Between 2007 and 2019, less than 10 projects funded by the European Research Council tackling COPD can be easily identified[32], with an overall budget of more than $12 million.[33] This indicates an annual budget of less than $1 million for the disease from the European Research Council. Overall, the 6 governmental funders I researched allocate between $86 million and $89 million towards COPD research per year.
A short search for other grantmakers in the field gave some results, including the Respiratory Health Association (less than $100 thousand in COPD research funding annually[34]), Asthma + Lung UK (previously Asthma UK and the British Lung Foundation, has given GBP3 million to COPD research over its lifetime), the American Lung Association (less than $0.2 million in COPD research funding annually), the American Thoracic Society (about $150 thousand in COPD research funding annually[35]), the Lung Foundation Australia (about $220 thousand in COPD research in 2021[36]), the CHEST Foundation ($30 thousand annually)[37], COPD Foundation ($5.3 million in COPD research in 2021[38]), American Respiratory Care Foundation, Canada’s Lung Health Foundation ($62 thousand in 2019[39]), and Canada’s Breathing as One ($120 thousand in 2020).[40] This amounts to an additional $7 million per year from philanthropic organizations (including funding by the Wellcome Trust).
Philanthropic and governmental actors contribute $95 million annually towards COPD research. It is likely that corporate funders add a significant amount of funding, however, I did not try to infer the level of corporate contributions as part of this essay.
Why should Open Philanthropy consider funding COPD research?
Above I have demonstrated the impact of COPD as a disease, as well as the fact that COPD research is neglected in terms of funding from both philanthropic as well as governmental sources. These two aspects of the topic (i.e. importance and neglectedness) can be stated with reasonable confidence, given the available data. Tractability, especially in regards to cost-effectivity of research funding, is harder to determine.
Cost and outcomes of biomedical research
Research about research is itself an underfunded field and, in my opinion, also deserves more attention from an effective altruism (EA) perspective, as more knowledge about the cost-effectiveness of biomedical research may convince more philanthropic funders that align with the EA mindset to provide funds to critical and underfunded research areas. Currently, our ability to estimate the impact of research funding is somewhat limited, but in the following I want to quickly present an easy back-of-the-envelope calculation to highlight how even slight health benefits from new medications may warrant large investments into research.
According to the Global Burden of Disease dataset, the global prevalence of COPD in 1990 was 115 million, compared to 212 million in 2019. This means if we assume linear growth of the patient population (which is obviously reducing complexity, as we ignore the equilibrium between death and new cases) about 3.3 million more patients are affected each year. Research investment today will have a substantial time lag to actual implementation and real-world health benefits. If we assume this lag to be 13 years, we would be dealing with about 266 million cases at the time health benefits occur (i.e. 2035). Let us just look at health benefits accrued over 10 years (i.e. treatment is disbursed to population affected at 2035 and new cases between 2035 and 2045). With an assumed benefit of 0.5 DALYs averted per person treated and a worldwide treatment coverage of 50%, this hypothetical treatment would avert almost 75 million DALYs. According to the 1000x bar of return on investment for Open Philanthropy, finding and disbursing such a treatment would warrant about $7.5 billion in investment (not including economic benefits of reduced disease burden).
This calculation is purely hypothetical and not based on any real-world data on the potential impact of COPD medication. For example, I believe that treatment coverage will likely lie well below 50%, as any targeted treatment is likely only applicable to a subpopulation of patients. Nonetheless, this calculation highlights the scale of COPD disease burden and how even a small effect size on the individual level can have large impacts overall due to the size of the patient population.
However, this is not to say that funding COPD research will necessarily pass Open Philanthropy’s bar for potential impact. Indeed, $7.5 billion is less than 10% of the current annual research budget for COPD and it does not seem like there has been much impact on disease burden during the last few years. The literature on the cost-effectiveness of research furthermore suggests that while funding biomedical research is often a good investment and cost-effective, it most likely does not pass the 1000x bar. For example, an analysis of the benefits from cancer research estimates the social value of improvements in life expectancy between 1988 and 2000 to be close to $2 trillion. While the researchers do not calculate a return-on-investment themselves, a short estimate puts this at about 25x (i.e. $2 trillion benefits versus a total budget of $80 billion for the National Cancer Institute between 1971 and 2000).[41] A similar study estimates the returns of publicly funded cancer research in the UK to be about 4x (or an internal rate of return of 10.1% in their words) when comparing expenditure on research between 1976 and 1995 (i.e. £5.3 billion) with health benefits gained between 1991 and 2010 (i.e. £124 billion with 17% of these attributable to research findings).[42] Overall, public investment into research is seen as more cost-effective than other public expenditures.[43]
Limitations
There are a number of limitations when estimating the rate of return of research funding. Basic research has a long lag-time between research taking place/findings being published and these findings being translated into clinical practice. The way we record research funding is adapted to administrative needs and not suited to calculate rates of return. One limitation that becomes clear in the examples presented above is that the time for which research findings impact health outcomes can differ vastly. For example, chemotherapies were developed in the 20th century but are still in clinical use today, allowing their development to impact healthcare for many decades and most likely making the funding that led to the discovery of chemotherapies highly cost-effective. On the other hand, some treatment approaches are only on the market for a few years before they are being replaced by better and more effective therapeutics, limiting their overall impact, and many other research findings never have any impact on the clinic.
Importantly, biomedical research is international and funding awarded in one country may generate health benefits across the globe. Furthermore, there will likely be differences in the average cost-effectiveness of different types of research (e.g. basic versus applied), but our current ability to differentiate seems to be limited. Despite these hurdles, there appears to be a push towards more accountability and funders seem more interested than ever to estimate the impact on their grants, including research funding.
Therefore, any estimates of rate of return mentioned here should be viewed with the limitations of the underlying methodology in mind. The same is true for the back-of-the-envelope calculation presented above.
Conclusion
To summarize, I am confident in the finding that COPD is a major public health issue and a highly underfunded area of research. Furthermore, it is fairly clear to me that additional funding in the space will accelerate the development of new and better treatments and, given the size of the patient population, even small health benefits can translate into large overall impact.
My assessment of cost-effectiveness of funding research into COPD (or research in general) is fairly shallow. While I have doubts on whether this funding opportunity can clear Open Philanthropy’s 1000x bar, the fact that the organization already funds biomedical research in its existing grant programs makes me believe that COPD research is a strong candidate for further consideration.
One point not mentioned so far, which seems to align with Open Philanthropy’s philosophy towards science funding (as demonstrated here[44]), is the fact that COPD is only one of many diseases that are driven by chronic inflammation and that there will be certain overlap between research into these conditions. Findings in COPD research regarding control of underlying inflammation may also translate to these other diseases, most of which remain without disease-modifying treatment options. Basic research into inflammatory conditions may also be more cost effective, as scholars have suggested that basic research, i.e. research aimed at learning how fundamental biological processes function, pays off in terms of key discoveries almost twice as much as other types of research.[45]
Where should additional funds go to?
As mentioned previously, there is limited data on the cost-effectivity of funding different types of research. There are a number of expert funders in the field that may have a better perspective on deserving and underfunded research areas and where funding may provide the most impact. These include existing funders such as Asthma + Lung UK, American Lung Association, Respiratory Health Association, and the COPD Foundation. However, based on a preliminary and shallow assessment of different kinds of research that may be worth funding, I believe there are a few topics that may deserve particular attention:
- Inhaled drug discovery: Research that increases our knowledge about drug properties required for optimal resorption through the lung can vastly enhance our ability to mitigate inflammatory and other processes in a lung-specific way.
- Inflammation: Understanding how inflammation is regulated and what makes inflammatory processes go awry in disease could lead to new and more targeted ways at preventing chronic inflammation in conditions like COPD (amongst many other).
- Patient heterogeneity: Discovering biomarkers and linking them to underlying pathogenic processes is an important step towards precision medicine. Identifying subpopulation of patients will bring us closer to understanding the heterogeneity of COPD and has the potential to make future clinical trials more effective.
- Steroid resistance: The development of steroid resistance is a major issue amongst COPD patients and may provide a ‘near-term’ goal that may be more tractable than developing disease-modifying therapeutics. A number of potential drug candidates are already known, but translation of these research findings is lagging behind.
Questions for further investigation?
- Does COPD research funding fulfill Open Philanthropy’s target for expected social returns?
- What are the most important and most effective research areas to target (both in terms of topics, as well as basic versus applied)? What are promising projects within these areas?
- How does funding COPD research compare to funding COPD prevention methods (e.g. tobacco bans and reduction of air pollution)?
- How effective could drug repurposing studies be for COPD and how well has this been explored in the past?
- What are major bottlenecks in COPD research and how could more funding alleviate these troubles?
- What are important topics in COPD research that were not covered in this shallow investigation?
- What is the potential health impact of disease-modifying COPD medication? With what probability and how long in the future could such a novel treatment be achieved?
- How likely is it that the pathogenic processes underlying COPD are not tractable by drugs in a meaningful way due to a large number of distinct pathways being at play?
- How important is capacity building and the attraction of talent for a research field?
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
It is slightly unclear how much overlap with other funding categories there are. For example, research regarding “certain diseases of the respiratory system” received $132.75 million in funding but it is unclear whether any or if how much of this funding also supported research work on COPD. While this may change funding levels, it does not change the overall conclusion that COPD research is underfunded.
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
https://erc.europa.eu/projects-figures/erc-funded-projects/results?search_api_views_fulltext=COPD (this is likely an underestimate as studies that did not mention COPD in their abstract were not included)
- ^
11926890 EUR
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^
- ^