First clean water, now clean air
By finm @ 2023-04-30T18:01 (+189)
This is a linkpost to https://finmoorhouse.com/writing/clean-air/
The excellent report from Rethink Priorities and 1Day Sooner was my main source for this (here’s a summary). Many of the substantial points I make are taken from it, though errors are my own. It’s worth reading! The authors are Gavriel Kleinwaks, Alastair Fraser-Urquhart, Jam Kraprayoon, and Josh Morrison.
Clean water
In the mid 19th century, London had a sewage problem. It relied on a patchwork of a few hundred sewers, of brick and wood, and hundreds of thousands of cesspits. The Thames — Londoners’ main source of drinking water — was near-opaque with waste. Here is Michael Faraday in an 1855 letter to The Times:
Near the bridges the feculence rolled up in clouds so dense that they were visible at the surface even in water of this kind […] The smell was very bad, and common to the whole of the water. It was the same as that which now comes up from the gully holes in the streets. The whole river was for the time a real sewer […] If we neglect this subject, we cannot expect to do so with impunity; nor ought we to be surprised if, ere many years are over, a season give us sad proof of the folly of our carelessness.

That “sad proof” arrived more than once. London saw around three outbreaks of cholera, killing upwards of 50,000 people in each outbreak.
But early efforts to address the public health crisis were guided by the wrong theory about how diseases spread. On the prevailing view, epidemics were caused by ‘miasma’ (bad air[1]) — a kind of poisonous mist from decomposing matter. Parliament commissioned a report on the ‘Sanitary Condition of the Labouring Population’, which showed a clear link between poverty and disease, and recommended a bunch of excellent and historically significant reforms. But one recommendation backfired because of this scientific misunderstanding: according to the miasma theory, it made sense to remove human waste through wastewater — but that water flowed into the Thames and contaminated it further.

But in one of these outbreaks, the physician John Snow has spotted how incidence of cholera clustered around a single water pump in Soho, suggesting that unclean water was the major source of the outbreak. A few years later, the experiments of Louis Pasteur helped foster the germ theory of disease, sharpening the understanding of how and why to treat drinking water for public health. These were well-timed discoveries —
Because soon things got even worse. Heat exacerbated the smell; and the summer of 1858 was unusually hot. 1858 was the year of London’s ‘Great Stink’, and the Thames “a Stygian pool, reeking with ineffable and intolerable horrors” in Prime Minister Disraeli’s words. The problem had become totally unignorable.
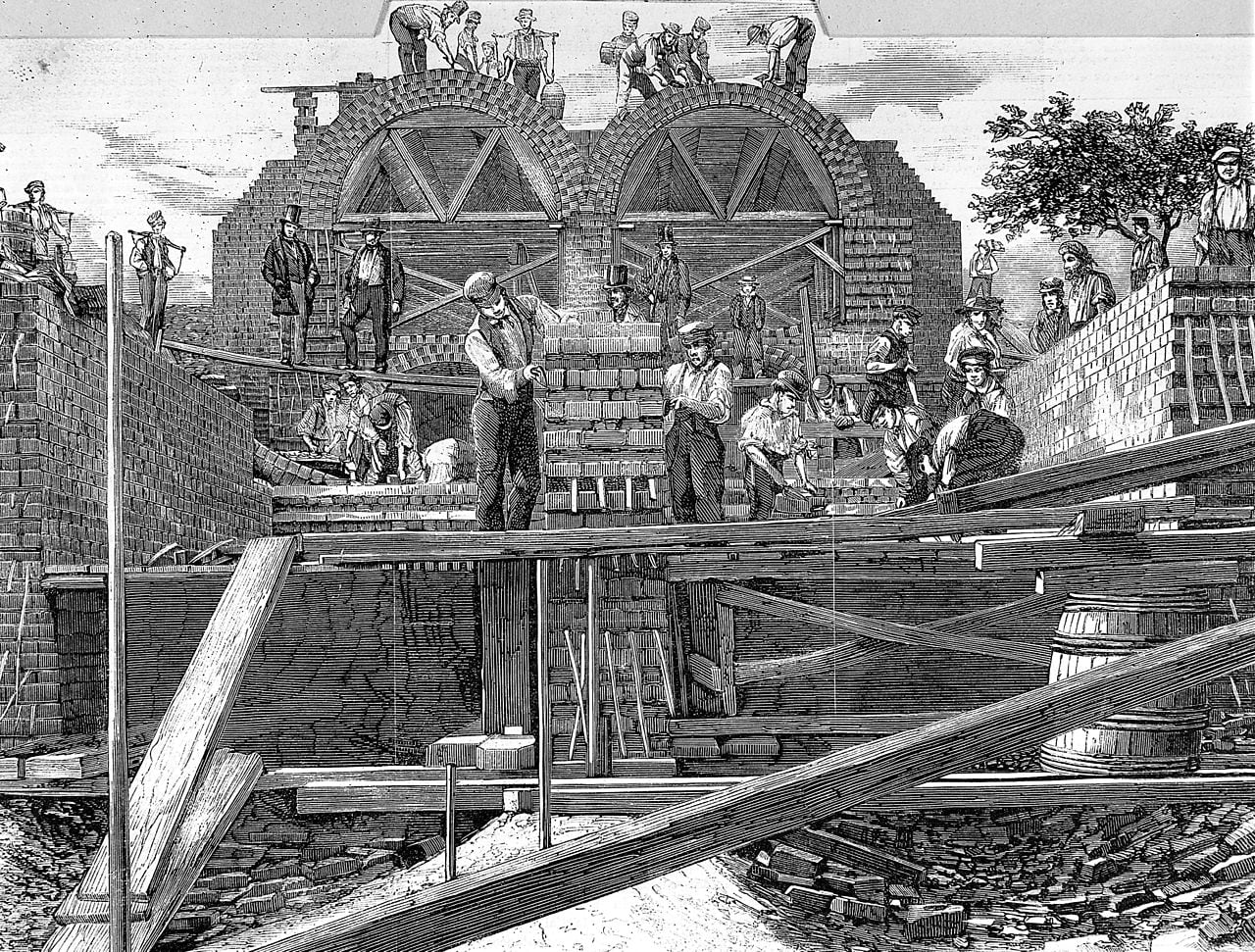
Parliament turned to Joseph Bazalgette, chief engineer of London’s Metropolitan Board of Works. Spurred by the Great Stink, he was given licence to oversee the construction of an ambitious plan to rebuild London’s sewage system, to his own design. 1,800km of street sewers would feed into 132km of main interconnecting sewers. A network of pumping stations was built, to lift sewage from streets below the high water mark. 18 years later[2], the result was the kind of modern sewage system we mostly take for granted: a system to collect wastewater and dump it far from where it could contaminate food and drinking water; in this case a dozen miles eastwards to the Thames estuary. "The great sewer that runs beneath Londoners”, wrote Bazalgette’s obituarist, “has added some 20 years to their chance of life”.
Remarkably, most of the system remains in use. London’s sewage system has obviously been expanded, and wastewater treatment is much better. Bazalgette’s plan was built to last, and succeeded.
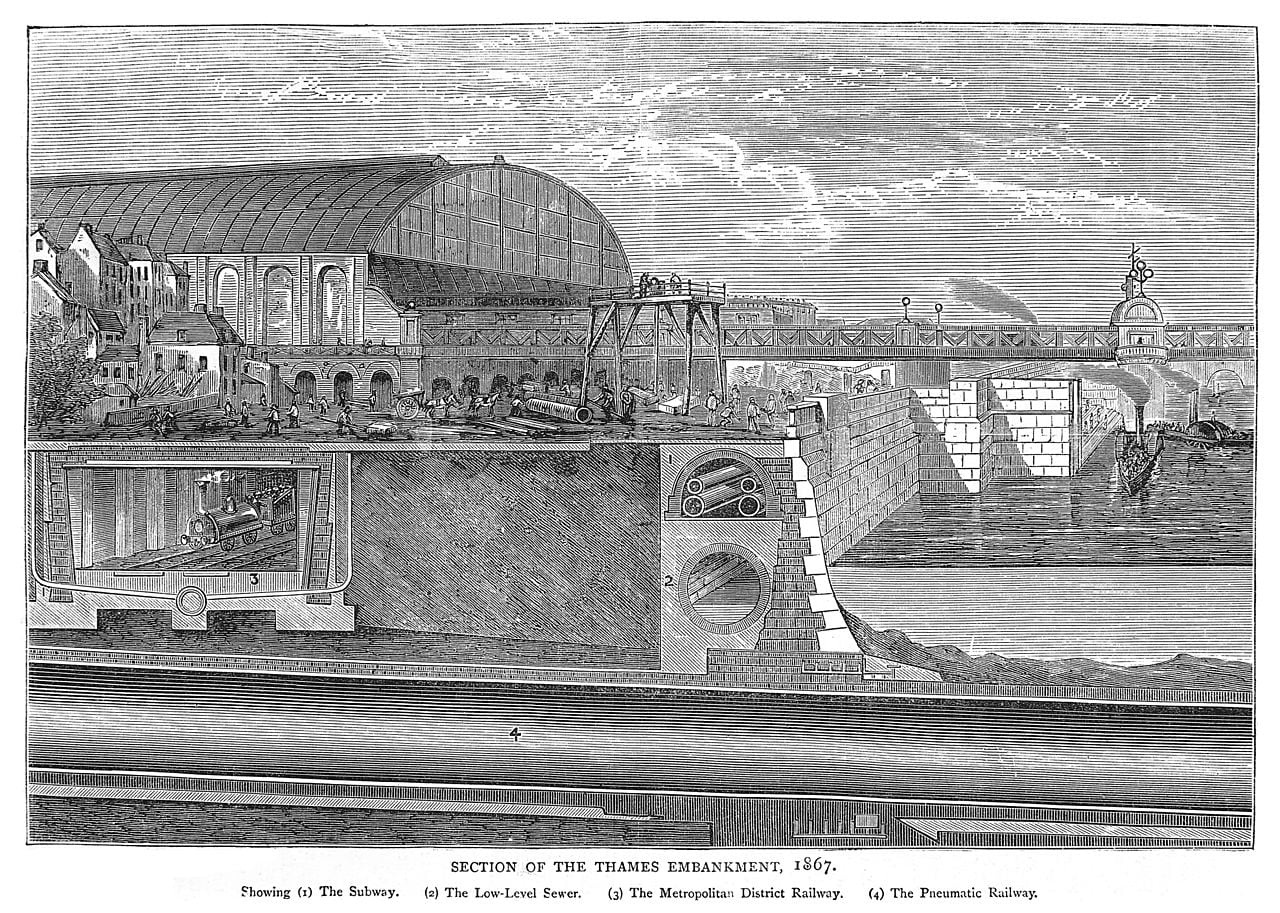
As London built ways of expelling wastewater, it also built ways of channelling clean and running drinking water. New canals, plumbing infrastructure, and water supply companies piped water from springs, wells, and rivers straight into houses and public drinking fountains; replacing wells, collecting rainwater, or unclean water pumps.
One of the nice things about living in London today is that it is very, very easy to find running water, and it’s reasonable to basically never worry about whether the water that comes out of taps is safe to drink. In the last century, 7 people have died of cholera in the United Kingdom.
The same story unfolded nearly everywhere in the developed world, and it marked the beginning of a so far effectively permanent end to waterborne disease in wealthy countries. I naively but conservatively estimate clean water measures saved more than 130 million people in the 50 years since 1973 alone.[3] Of course these improvements to sewage and plumbing and water treatment were expensive, but very clearly paid for themselves many times over, and it is clearly worth expanding those measures until everyone in the world has access to them.
That’s not mentioning the improvements from sanitation and hygiene, which are different from just having access to clean drinking water. Unsafe sanitation and lack of access to handwashing facilities, treated as risk factors, together look responsible for nearly 1.5 million additional deaths annually.
I just think this is worth dwelling on: in about half a century, developed countries effectively ended waterborne disease.
Clean air
You probably guessed from the title but the punchline is that now’s a good time to do the same thing with airborne disease.
The basic analogy:
- Unclean water imposed an enormous human toll, until we built ways to deliver clean water, dispose of unclean water, and keep the two separated. Now nearly everyone in at least developed countries has access to safe drinking water, and in those places most waterborne diseases are very rare.
- Unclean indoor air continues to impose an enormous human toll, even in developed countries. Almost nowhere in the world do we adequately treat, monitor, or even circulate the air we breathe: we breathe untreated air pretty much all the time. But we know how to build measures to effectively end airborne diseases, too.
I think the first step here is just noticing the price we pay for unclean indoor air. Consider: most people just have to factor in a ~single digit number of days per year recovering from some airborne disease like the flu or common cold. In the US alone, this costs double-digit billions of dollars in direct healthcare costs and foregone wages. Ventilating air helps to eliminate biological pathogens, but it also just makes it fresher and less stuffy — where some studies tentatively show double digit percentage improvements in productivity from just getting rid of stuffy (CO2-rich) air. But likely the biggest cost is now also the most obvious. Every few decades a pandemic with airborne transmission pathways will tear through the world, and the world will be mostly powerless to stop it. The most recent example took around 20 million lives so far. The next could be even worse.
Part of the problem with making these facts salient might be that our disgust reactions aren’t firing in helpful ways: unclean water is visibly (and olfactorily) unclean, but bad air is perfectly disguised as clean air, and contextual cues are needed.[4] So the first step is bringing the human costs of unclean air into the open.
In the hopeful story, these costs become historical. Covid could be to airborne diseases like London’s cholera outbreaks and Great Stink were to waterborne diseases: a confluence of (i) “wow, as long as we know how to end this, we should”; and (ii) “huh, looks like we do increasingly know how to end this”.
I don’t know whether that is the story we’re in, but I think we know enough to describe many of the practicalities. So here’s how the hopeful story could play out, across a handful of technologies:
The high-level plan
We’ll focus on indoor air quality, because respiratory pathogens are much more likely to spread indoors than outdoors[5] (and treating indoor air is achievable and affordable).
The world we want to end up in is a world where we massively slow the spread of airborne pathogens, primarily to reduce the vast expected cost of catastrophic biorisk, and also to reduce the yearly toll of (non-pandemic) respiratory diseases.
How do we reach that point of safety? Practically, we’ll need technology that does two things. Either: straightforwardly blocking the spread of pathogens in crowded indoor spaces. If patient zero coughs, and the aerosolized pathogen is sterilised or ventilated away before it can spread to anyone else, then a potential outbreak is stopped dead. Or, at least: slowing transmission. If R0 drops and stays below 1, you don’t have the conditions for an epidemic. And in any case, slowing transmission buys time for other medical countermeasures — like the time to develop and deploy vaccines.
On a social level, we’ll need ways to make sure these safety-promoting technologies are deployed as widely, cheaply, and quickly as they need to be. With two tools: (i) standards and other regulations to capture the externalities from unclean air; and (ii) major R&D initiatives like prizes, FROs, or advanced market commitments to speed up wide rollouts of these safety-promoting technologies.
Which technologies?
Ventilation
Ventilation just means getting rid of the stale air in a room and replacing it with air from outside the room. If the air from outside the room is cleaner, then you’ve now got cleaner air.
This metaanalysis finds strong evidence that ventilation helps reduce infection rates. There’s also some evidence for more general health benefits, like less inflammation, sick leave, and fewer asthma and allergy symptoms.
The V in HVAC is ventilation, so many AC / heating systems ventilate air already. A DIY version of a ventilation system is to open two roughly opposite windows in a space, and place a fan moving air out one of the windows.
There are some drawbacks: it’s often noisy, often energy-consuming, and it relies on outdoor air being significantly fresher than indoors, which isn’t always the case (especially in cities).
Filtration
Then there’s filtration: passing air through a filter to remove small particles, including pathogens. Quoting from this Rethink / 1Day Sooner report on indoor air quality:
Standalone filtration units […] have been shown to reduce the exposure to pathogenic aerosols under controlled conditions, with 5 eACH HEPA filtration in classrooms enough to cause a 4-5 fold drop in pathogen dose.
[…] Addition of filters to existing ventilation systems in a typical model scenario has been shown to reduce relative risk of infection of influenza by up to 47%, at a total annual cost of $352 for HEPA filters[.]
[…] In addition to reducing pathogen transmission, filtration has benefits for respiratory health and cognition, due to its ability to remove harmful particulate, gaseous, and chemical pollutants. Given these benefits, widely investing in improved filtration in built environments is likely to help the population even in non-pandemic years.
The way filters work — even the advanced ones — is almost embarrassingly simple. Get some kind of foamy/spongy/fibrous material with lots of small holes; put many layers of that material into a box; and force air through that box with a fan. During the pandemic, Richard Corsi proposed a design for a DIY air purifier which is more or less as simple as I made out, enabling people to cheaply build their own air purifiers for homes and schools and offices. It’s called the Corsi-Rosenthal box, and it takes about $100 and 15 minutes to build. Here is Corsi in a radio interview: “People are now reporting 600 cubic feet per minute (280 L/s) in clean air delivery rates. That’s phenomenal. That’s actually better than a lot of the more expensive HEPA-based portable air cleaners”. Even more than ventilation systems, air filters are low-tech, and already very cheap to install and maintain (I’d guess typically less expensive than fire safety systems).
An aside: ventilation plus filtration is the major reason that the risk of Covid infections on flights was and is so relatively low: air in the cabin is replaced every couple minutes, fresh air is drawn from outside the plane, and mixed with recycled air passed through HEPA filters. Airbus says that the risk of infection is lower on a plane than people sitting six feet apart in an office.
Ultraviolet germicidal irradiation (UVGI)
Like antibacterial soap, it turns out that certain wavelengths of light can effectively sterilise pathogens (without sterilising humans). There are roughly two kinds:
Upper-room UVC illuminates the top of the room and avoids illuminating people. This means you can use relatively lower frequencies of UV light which are currently easier to produce with lamps, but which can cause eye damage in humans. Upper-room UVC is cheap and well-understood. This study found an 80% reduction in TB transmission in guinea pigs. So it will also keep pets safe.
Far-UVC is a narrow band of UV wavelengths at higher frequencies than are currently economical to produce with lamps. The key advantage of Far-UVC is that early studies show no indications that it harms humans, even at very high doses. But it is effective at stopping pathogens: for example this study finds that Far-UVC light inactivated 99.9% of aerosolized coronaviruses. As long as longer-term studies on the safety of Far-UVC agree, then this is some extremely exciting technology.
Currently, Far-UVC is too expensive to scale to a significant fraction of all the indoor spaces in a country. We’ll need a few years of figuring out how to produce it more cheaply (ideally with LEDs).
In the hopeful story, new PhDs and R&D labs begin a concerted program to first make the breakthroughs which would enable Far-UVC to become cheap, and then major manufacturers introduce the technology to wider and wider markets. It might parallel the story of solar photovoltaic tech[6]: between 1975 and 2021, the cost of a watt of solar energy fell by more than 40,000%; and by more than 600% in the past decade alone. The process from now to real maturity — where Far-UVC is cheap enough to be ubiquitous — needn’t last much longer than Bazalgette’s 18-year sewage project.
Standards and monitoring
The expectation of clean water in wealthy countries is enabled by technology and infrastructure; like effective sewage systems and water treatment facilities. But to a large extent it is also enabled, and was initially bootstrapped, by sound policymaking and regulation.
Regulation requires verification. In the UK the Water Supply (Water Quality) Regulations 2016 say things about how much lead can be in my tap water (< 10µg/litre), and water test kits exist to check for lead concentrations, giving those regulations teeth. Similarly, UK building standards say things about how new builds should handle drainage and waste disposal and other exciting things, all easily verifiable.
So is it easy to measure air quality? Pretty much. The concentration of CO2 in a room can be a good proxy for how well ventilated it is (and therefore for risk of transmission without filtration or germicidal light). Plus, CO2 buildup itself can be cognitively impairing. CO2 monitors can cost less than $20. Only a notch more expensive are gauges for different sizes of particulates. Again, particulate matter in general can both proxy well for the effectiveness of filtration, and cause breathing problems of their own. Metagenomic sequencing technology could also survey the air for actual pathogenic material, but it needs to become cheaper first[7]. So we have multiple easy ways to measure air quality, which is good news for straightforward, boring, scalable kinds of air quality guidelines[8].
Think about water safety regulations again: I don’t really know what they say, and I don’t need to. I just trust that they make sure the water that comes out of my taps is safe. I imagine the story where we achieve a world of clean indoor air would look similar.
Some places where it might be possible to make near-term improvements to regulations and guidelines:
- The WHO Guidelines for Indoor Air Quality mention dangerous chemicals and gases, but not particulate matter or (crucially) pathogens and their transmission potential
- Most buildings in the US fall under ASHRAE Standards 62.1 and 62.2, which do not consider airborne pathogens
- The Occupational Safety and Health Administration in the US can regulate indoor air in workplaces, but its regulations are a little thin on the ground, don’t mention pathogens, and rely on self-certification in most cases
- Encouragingly, the Biden administration announced initiatives to support clean indoor air, including a revised “Clean Air in Buildings Challenge” listing a bunch of sensible suggested upgrades to air quality, and offering funds from the American Rescue Plan and Bipartisan Infrastructure Law funds. But funds could be more explicitly earmarked for this purpose, as they were planned to be in the Pandemic Preparedness Plan (AP3) which did not pass
Thinking further ahead with a wealthy country like the US or UK in mind, we might imagine:
- Air quality guidelines have been introduced, plus the means to easily monitor air quality. Subsidies are set up for adding filtration, ventilation, and even UVC into homes and workplaces. More robust standards[9] are established for new builds
- As a consequence, much like how plumbers will fit houses to a boiler by adapting some of the plumbing, there are also services to adapt houses for cleaner/sanitised air; such as by installing a system of air ducts, rather than just putting a HEPA filter in the corner of a room
Getting started
When we have such a successful precedent in the story of clean water, there is something so transparently worthwhile about this prospect of creating clean indoor air.
I’m not sure I emphasised this enough: if a country installed all the measures I mentioned, it could more or less end respiratory disease in that country. A world in which clean air measures are as widespread as clean water measures are in rich countries is a world which has effectively ended respiratory disease everywhere. It’s just totally possible to stop worrying about a relative catching a cold, or the flu, or pneumonia.
That’s a huge deal: ignoring pandemics, even halving deaths from respiratory disease means saving hundreds of thousands of lives every year. Not ignoring pandemics, the numbers are of course much starker. It’s hard to quantify how bad truly worst-case pandemics could be, given that they could have civilisation-spanning consequences. But these basic measures would help stop or slow many of them.
Like with waterborne diseases, the wealthiest countries will probably get there first[10]. A ballpark upper-bound estimate for the cost of comprehensively installing the measures I’ve described in buildings across the US is about $200 billion, or about $50 billion for a more targeted program focusing on buildings like schools and hospitals. But this would surely be worthwhile: even in economic terms, it would save tens of billions in healthcare costs, tens of billions of dollars from lost productivity due to illness, and further further tens of billions from the continued risk of another pandemic (see the appendix on costs).
But we needn’t rely on government spending forever and for every part of the plan. Technologies become cheaper when people build lots of instances of them. To give one example, there may come a point where Far-UVC technology is affordable enough to past the cost-benefit test for businesses looking to protect their employees from disease. This is win-win-win territory: employees would prefer to work in an environment where they don’t get semi-regularly sick; employers benefit because fewer employees get sick; and the world benefits because that is one less office-sized petri dish spawning airborne disease for everyone else. In many cases, it’s about supporting a one-time lift to get to that self-sustaining state where everyone’s incentives are aligned.
In short: practical measures to improve indoor air quality seem like an historically good deal.
The story of spreading access to clean water and sanitation is not over. Unsafe water causes more than a million deaths a year — the 13th leading risk factor on one way of slicing things up. Almost all the deaths from unsafe water are concentrated on poor countries, especially sub-Saharan Africa and India. And a solid 25% of the world lacks access to safely managed drinking water. But full access to clean water is no longer encumbered by knowledge about how diseases spread, or how to properly treat water: we have the blueprints. We know how to bring this story to a happy, if belated, ending.
If the project of spreading access to clean water, then let’s do the same for clean air. What’s stopping that from happening? Surely not that it’s impossibly expensive: the cost-benefit analysis already tips in favour for many countries. Nor feasibility: we either already have the technology at scalable prices, or we have clear precedent for similar technologies plummeting in price with R&D. So maybe what’s stopping the story repeating are things like awareness, political will, the visibility of early adopters, and funding for foundational research. And — hopefully — those things are changeable.
More links
- Air Safety to Combat Global Catastrophic Biorisks — Rethink Priorities and 1Day Sooner
- The Plan to Stop Every Respiratory Virus at Once — The Atlantic
- A paradigm shift to combat indoor respiratory infection — Science
- Pandemic prevention as fire-fighting — Works in Progress
Appendix: other ways to stop pandemics
I’ve described what it could look like for the world to get its act together on indoor air quality, and begin to deliver clean air at scale, just how most countries in the world deliver clean, safe water almost universally.
A major motivation for caring about this is that such a plan could help end respiratory pandemics. But it’s really worth noting that these aren’t the only tools we have (and which the world at large seems to be underrating) to end that threat. Rather, provisions for clean air would complement other strategies to reach a world which is effectively immune to catastrophic pandemics. Here’s a quick and non-exhaustive list:
- We could develop upgraded ultra-safe PPE, e.g. with air purifying respirators, which is comfortable to keep on for many hours at a time. We can stockpile enough of these systems to enable essential workers across the world to keep basic services running in a worst-case pandemic
- We could build a world-spanning network for detecting novel and pandemic-capable pathogens as they emerge, even when the signs are subtle. Pathogen-agnostic sequencing technology can be installed to monitor wastewater in populous areas, and as it becomes cheaper it could even begin monitoring the air in busy public buildings with high throughput; ready to pick up on known and unknown pathogens
- We could build the capacity to develop and deploy vaccines, and hand out flexible or universal tests to everyone; curbing human-to-human transmission
I think these measures — especially better PPE and sequencing — could be even more important than the clean air measures I’ve described for stopping worst-case pandemics, because of how specifically effective they could be for that class of threat. But again, these are complementary rather than exclusive options.
Appendix: costs and benefits
Taking indoor air quality seriously would mean spending billions of dollars annually for at least a decade or so. So let’s get quantitative.
First, the costs. Focusing on the US, this report from Rethink Priorities and 1Day Sooneerstimates that upgrading the air quality systems in all commercial buildings (at current technology costs) would add up to ~$214 billion total, or ~$10.1 billion focusing just on healthcare facilities and hospitals, or ~$39.2 billion focusing just on offices. On the most widely-used measure[11], upper-room and far-UVC[12] look the most cost-effective[13], with operational costs less than 20% of ventilation and filtration. I get an estimate of about $78 billion to install Upper-room or far-UVC in every hospital, healthcare facility, and K-12 schools[14]. So the headline costs for installing the clean air interventions I’ve described are something like: roughly $50 billion if you’re focusing on the most vulnerable, high-priority public spaces; and roughly $250 billion for a more comprehensive plan. Those estimates are more likely to be conservative than much too high, because they don’t anticipate that costs will fall significantly from today-prices, and they totally could.
Can we try pricing the benefits? The same Rethink Report makes a rough estimate that plans on the more comprehensive end of what I’ve described could reduce overall rates of transmission of respiratory disease by just under 70%.
First, there’s the cost from non-pandemic transmissible diseases. This breaks down to the morbidity cost of not being able to work (lost wages), the direct cost of healthcare, and in worst cases the mortality cost. This 2000 report estimates that infectious diseases account for 15% of US healthcare spending, which in 2020 accounted for about 14% of US GDP (combining public and private spending). US GDP is about $23tn. Let’s conservatively guess that 10% of that burden could be eliminated by properly treating and sanitising indoor air and surfaces. That would suggest a saving from the direct healthcare costs of $23tn × 15% × 14% × 10% = roughly $50 billion. Figuring out lost wages is tricker (I couldn’t find a direct estimate in 10 minutes of looking). The ONS suggests that the sickness absence rate in the UK is about 2%, which we can assume is roughly the same in the US. Let’s again assume that 20% of these sick days could be prevented by significantly upping our game on killing germs in indoor spaces. And we’ll assume that the elasticity of total working days to GDP is about 0.2 (increasing working days by 1% increases GDP by 0.2%). That gives a BOTEC of the losses from diseases preventable by fixing indoor air and surfaces of: $23 trillion × 2% × 20% × 0.2, which roughly equals $20 billion.
Then there’s pandemics. The Institute for Progress estimate the overall cost from Covid to the US at around $10 trillion. Conservatively assuming a yearly likelihood of a pandemic at least as bad as Covid of 2%, that suggests the US faces a yearly expected cost from the risk of pandemic per year of at least $200 billion. The amortised annual cost of the program we’ve described would be about $20 billion per year for a decade or so, meeting the cost-effectiveness bar if it reduces that risk by at least 10%[15].
That’s not mentioning the costs from impaired cognition caused from poor air quality; or the cost to health from non-pathogenic matter like small particulates. I’m still a bit confused by the literature on cognitive costs of poor air quality, but it seems like the effects of stuffy indoor air on day-to-day productivity are real and possibly quite large. This study assessed the effect of C02 concentration on performance on tasks designed to measure “complex cognitive functioning in ways […] relevant to the tasks of workers in buildings”. Eyeballing the results, it looks like the drop in performance from relatively clear air (600ppm) to a fairly stuffy office (1000ppm) led to a 11–23% drops in the raw scores on these tests (about 15% on average), and the drop from fresh air to ~a very stuffy meeting room (2500ppm) ranged from 44 to 94% across the tasks. N=22 and I’m coming at this with a skeptical prior, so I’d guess the real effects of C02 are smaller. But if they’re in the same ballpark, then there are some huge gains to be made for just making sure indoor air is fresher, on the order of billions of dollars in productivity gains in the US. You can see more discussion on this LessWrong post, including this mini literature review from Gwern. This study and this review also find significant effects.
If the spending numbers sound like a lot, consider how much the US is prepared to spend on fire safety: around $273 billion in 2014. And the majority of that spending is directly comparable to the air quality improvements I’m discussing: things like installing sprinklers, installing alarms, and using fire-resistant materials in buildings and products. Covid alone caused five times more deaths than all fires in the last 45 years combined. The implication is not that we’re overspending on fire safety (not sure if anyone holds that take strongly) but that if it is worth it to spend hundreds of billions on fire safety measures every year, then it’s probably worth doing the same for indoor air quality measures. Or consider that the US is prepared to spend well over $500 billion annually on defence spending (relevant because defence against pathogens is also a kind of national defence). Or more than $200 billion annually on counterterrorism over the past decade or so.
Speaking more speculatively: I see a significant difference between spending on clean air on one hand, and examples like fire safety, counterterrorism, and national defence (military) spending on the other: externalities. If the cost to install e.g. far-UVC in a workplace falls, then it’s easy to imagine an increasing number of workplaces becoming willing to pay the full sticker price, just to recoup the opportunity cost of sick leave (and because employees might begin to demand that their working environment isn’t one where they’re exposed to a constant risk of getting sick). For potential buyers willing to pay less than the sticker price to install clean air measures, a government would only have to subsidise the difference to buy all the externalities (like all the people going home from work not spreading disease on the subway). By contrast, a business is unlikely to choose to donate to their local fire station out of sheer self-interest, because they’d capture too small a fraction of the benefits.
- ^
The same idea gave us the word ‘malaria’, also literally ‘bad air’ through medieval Italian
- ^
Many of these facts are from The Good Ancestor (2020)
- ^
The Global Burden of Disease estimates that unsafe water sources are still responsible for 1.2 million deaths each year. Very roughly three quarters of the world have access to a clean water source, and 6% of the world population did not have access to an improved water source of any kind. So let’s conservatively guess that clean water measures reduce the deaths attributable to unsafe water by 75%, compared to a world with the same population but no clean water technology, on average from 1973 to the present day (i.e. over the last 50 years). In other words, we’re guessing that without clean water measures, deaths from unsafe water would be $1.2 million / (1-75%) = 4.8 million and so counterfactual lives saved per year is 4.8-1.2 = 3.6 million per year. Average world population over that period was about 75% of today. So a naive and conservative guess at the lives saved from clean water measures = 75% × 3.6 million × 50 = 135 million people.
- ^
Obviously this changed some during the pandemic. For instance, sitting in a packed subway train (without a mask) still feels mildly stressful.
- ^
Largely because indoor spaces are more crowded. This study estimates more than 90% of Covid infections occurred indoors.
- ^
In a nutshell: (1) Solar cells were pioneered in R&D labs, often backed by governments. E.g. the US wanted to put solar cells on spacecraft; (2) Then they began being sold to private buyers in niche markets. E.g. Japan subsidised solar cells for calculators, toys, and watches; (3) Then Germany began a major subsidy program to develop domestic solar power capacity in the early 2000s; (4) Then other manufacturers took the grid energy solar tech and drove down costs through building a ton of it; especially in China. As a result, between 1975 and 2021, the cost of a watt of solar energy fell by more than 40,000%; and by more than 600% in the past decade alone. Solar PV also did not majorly benefit from philanthropic funding, in the form of e.g. prizes or advanced market commitments. So it’s a story which demonstrates how costs can fall quickly and dramatically with (i) major investment and (ii) the ability to learn from building millions of units (unlike e.g. nuclear power plants). Both those factors can apply to Far-UVC, and we have the option to supercharge the process with early incentives.
- ^
There will presumably be a point where the sequencing technology is affordable enough to be used in some government standards, but too expensive to be permanently installed in most businesses / buildings / homes. In this case, you could imagine inspectors who visit on the order of every couple years to take samples of air from buildings, and mandate changes (e.g. some government subsidised filtration system) if the readings are bad (analogous to fire safety inspections).
- ^
One nice common feature of having widespread air quality measurement is that people can learn instincts and norms around improving air quality. For instance, some people who use CO2 monitors eventually become more sensitive to when a room feels ‘stuffy’, and when a room appears poorly ventilated such that they can expect it will feel stuffy. Similar to how people became more sensitive to shaking hands or touching one’s face once those things were made salient as ways to transmit Covid and other diseases.
- ^
Niche building regulations: who said effective altruists can’t dream!
- ^
Frontier R&D tends to be concentrated in rich countries, and rich governments are going to be more able to afford expensive public health programs. But also: if utility is sublinear with consumption, then people will be willing to spend relatively more on their safety as they become richer.
- ^
The measure being ‘equivalent air changes per hour’, or eACH. Air changes per hour is just a measure of how often air is recycled in a room. UVC doesn’t literally recycle air, but it does make the air cleaner, so the effect can be compared.
- ^
Assuming the costs of far-UVC fall to become roughly comparable with upper-room UVC.
- ^
Considering the amortised cost of installing and running mechanical ventilation; i.e. in terms of both installation and maintenance.
- ^
Total US building stock is ~340 billion square feet, of which ~7% are K-12 schools (assuming half of all floorspace used for education) and ~4.7% is for hospitals/healthcare facilities. Assume an installation cost of ~$1500 per ~70m2 room (per this source which gives an estimate for upper-room UVC, and assuming far-UVC falls to be comparable). Multiplying together gives ~$78 billion.
- ^
Another angle: the expected cost to the US from one percentage point of risk of a pandemic at least twice as bad occurring within a given time period (say 50 years) is at least $200 billion. It seems entirely plausible that the program described would reduce that cumulative risk by at least a percentage point for around $200 billion.
Gavriel Kleinwaks @ 2023-05-03T19:22 (+15)
Thanks so much for the kind words about our report! We actually published an updated version just an hour ago--you can see the new report here and the forum announcement with a summary here. (Small note on organizational affiliation: the report is a collaboration between 1Day Sooner and Rethink Priorities.)
ezrah @ 2023-05-04T07:28 (+10)
Excellent post, and great work on the research report!
From a narrative perspective I think the analogy between Clean Water and Clean Air is great. However, I'm wondering if from a R&D and implementation perspective a more fitting analogy would be clean cooking fuel, heating or solar power (which you do mention). Clean water systems need large investment in infrastructure and government implementation upfront, as much as they need more technological advancement, since Clean Water is a public good. Indoor Clean Air, or at least the solutions you described above, don't need large infrastructure or government investment. The quality of the air in my house or office is a private good. The private market can develop the R&D and market directly to consumers, without the need for the government to step in, as long as there's consumer interest.
The fact that the TOC for Clean Air Indoors doesn't need to go through government makes me more optimistic about success (although of course if there are government standards and gov R&D spending, it will go faster).
On the other hand, perhaps Indoor Clean Air is more similar to lead paint regulation, where the individual consumer isn't aware enough of the dangers and benefits, even though theoretically it's more lucrative to sell safe paint than poisonous paint.
Max Görlitz @ 2023-05-02T15:02 (+9)
Great post! I also believe in the need to get our air clean ASAP.
Self-promotion: check out SecureBio's work on far-UVC. We will hopefully publish more write-ups soon.
Minor point: In an informal survey of experts in the field, most people preferred the term germicidal UV (GUV) over Ultraviolet germicidal irradiation (UVGI). I also think that UVGI is a bit unwieldy, and "irradiation" sounds scary (although in Rethink Priorities' survey on this, the name didn't seem to matter much for people's impressions of the technology).
Interesting observation: With indoor air cleaners, there doesn't seem to be any real-world epidemiological evidence of whether they reduce infection rates (of course, on priors, I would expect them to). At least I didn't find any studies when I looked into it a few months ago, which surprised me. Such data also doesn't yet exist for far-UVC, but there is a bunch on conventional upper-room GUV (most of it decades old, though).
Good news on the regulation side: ASHRAE Commits to Developing an IAQ Pathogen Mitigation Standard. I'll be curious to see what comes out of it.
Also, I have a standing invitation for people to contact me if they are interested in working on GUV or far-UVC specifically and want to know what they could do!
Lizka @ 2023-04-30T22:21 (+8)
Thanks for sharing this! Curating. I'd be excited to see more essays that dive into the histories of how societies accomplished something analogous to what we might want to do — or attempt to answer questions like: "What's something that seems ~normal to us that future people might think was a constant tragedy or unnecessary problem until it was ~solved? How do we solve this?"[1]
I also really appreciated the back-of-the-envelope calculations for backing e.g. claims of cost-effectiveness (see e.g. the estimate for lost wages in the appendix on costs and benefits).
Assorted other notes and questions:
- I initially thought this would be about air pollution, which also seems like a very promising area for work. If you think it's important to avoid the misconception, you could change the title.
- Re: "Part of the problem with making these facts salient might be that our disgust reactions aren’t firing in helpful ways: unclean water is visibly (and olfactorily) unclean, but bad air is perfectly disguised as clean air, and contextual cues are needed. So the first step is bringing the human costs of unclean air into the open." I thought the emphasis on the visual aspect was interesting! And it seems plausible, so I'd be interested in testing the hypothesis as if it's true, it seems like there's a potential for advocacy through things like visualizations. (I still remember e.g. the NYT's 3D visual of particles spreading in a room (paywalled), and there's also this piece on school ventilation (also paywalled).[2])
- I noticed that I was tempted to check how much I agreed with a bunch of claims in the essay — like the implication that 2%/year is a conservative likelihood for a pandemic as bad as COVID ("Conservatively assuming a yearly likelihood of a pandemic at least as bad as Covid of 2%").[3] There are a lot of (sub)claims in the essay and I expect that I'd disagree with some if I started checking, but I mostly think this is due to a virtue of the post; the claims are easy to argue with.
- It seems useful to re-emphasize that improving air quality to slow (or stop) the spread of airborne diseases in richer countries seems to just make sense from those countries' perspectives, even setting aside benefits to the rest of the world. (This is quite compatible with the approach taken in How much should governments pay to prevent catastrophes?)
- I appreciated this note:
- "The story of spreading access to clean water and sanitation is not over. Unsafe water causes more than a million deaths a year — the 13th leading risk factor on one way of slicing things up. Almost all the deaths from unsafe water are concentrated on poor countries, especially sub-Saharan Africa and India. And a solid 25% of the world lacks access to safely managed drinking water. But full access to clean water is no longer encumbered by knowledge about how diseases spread, or how to properly treat water: we have the blueprints."
- ^
A relevant part from the post:
...the first step is bringing the human costs of unclean air into the open.
In the hopeful story, these costs become historical. Covid could be to airborne diseases like London’s cholera outbreaks and Great Stink were to waterborne diseases: a confluence of (i) “wow, as long as we know how to end this, we should”; and (ii) “huh, looks like we do increasingly know how to end this”.
- ^
- ^
This doesn't sound crazy to me, but I want to check it for myself (or find a link that seems credible). I decided not to continue down the side-quest right now in the interest of time, but would be interested.
MathiasKB @ 2023-05-01T12:14 (+7)
I'm convinced, what needs to happen for institutions such as the US HHS or European Commission's dg HERA to take on these initiatives? To what extent are they already?
I would suspect that one of the bottlenecks may be cheap and well-formulated plans. Good arguments can go far in policy, but I imagine success requires going from "We need UVC/Ventilation in every hospital" to "Try this specific pilot scheme to test efficacy".
Which are the pandemic preparedness organizations working on getting wins around the world? If eg. Denmark adopts Far-UVC and it is a smash success, it becomes a lot easier to advocate for elsewhere. My impression is that many of the EA organizations doing advocacy, mostly are doing it at the broader level of "we need better biosecurity" rather than proposing and pushing for very specific plans. Is my impression correct, or am I just not sufficiently familiar with the field?
Gavriel Kleinwaks @ 2023-05-03T19:35 (+4)
Great questions--my colleagues and I (at 1Day Sooner) have actually spoken to representatives from HERA and BARDA (which is under HHS) who are very interested in the potential of far-UVC. What we've seen is that policymakers are genuinely concerned about the effectiveness and safety of widespread far-UVC use, and want to see greater research in the field, without necessarily being able to guarantee that funding themselves. We, and other organizations, have been advocating for and trying to organize research and pilot programs. (I don't have a good sense of the international advocacy field around pandemic prep, though; most of our partners are based in the US.) I think that generally advocacy has actually been fairly specific, or at least been targeted at understanding specific concerns from policymakers, but it's not surprising that this doesn't necessarily come across at a glance. The more detailed and specific the plan, the more technical it gets and the more it's being communicated person-to-person or through gigantic reports. Our report does contain specific recommendations in the "Bottlenecks and Funding Opportunities" section if you'd like to check it out!
jvb @ 2023-05-09T16:26 (+4)
We (the biosecurity team at Convergent Research) also have curated a number of specific, tarmac-ready far-UVC projects with teams and timelines attached, that range from a few 100k to a few million and address various bottlenecks in far-UVC adoption. We've got a whole catalogue of 1-pagers if any funders reading this are interested :P
I think I have a slightly different read on USGOV's interest in far-UVC than Gavriel does. ~Every agency we've spoken to so far has gone "cool, but not our problem," which I understand to mean that far-UVC is not being prioritized even within the already-deprioritized category of pandemic funding. Hell, even NIAID isn't interested. This might change, of course...but no real idea of what might be a turning point. That being said, the CDC doesn't seem actively unfriendly to the tech, so there is hope?
Connor Tabarrok @ 2023-05-10T15:05 (+5)
Hi! I'm a water resources engineer by day, so this post caught my eye. There are tons of parallels to be drawn here between water treatment and air treatment, and I think you've done a great job outlining the scale of potential benefits available to us. However, some key differences arise in how we interact with air and with water in our daily lives. The water supply chain is cordoned off from other environments and the larger global supply of water, meaning we can take small volumes relative to the total supply and apply targeted treatment techniques to improve the quality of the consumed volume. With regards to air quality, much of our consumption is still directly from the global supply (the atmosphere). While we do have systems in place to filter and treat this air indoors, outdoor air quality is a much larger beast to tackle, and it may be more efficient to opt for intervention at point of consumption, in the form of masks/aerators, than to attempt to treat the global air volume. Turning to pathogenic risk, I think you've correctly identified an area of great potential improvement, since most airborne pathogenic transmission happens indoors, where we could conceivably intervene via existing AC / air supply systems.
Both of these measures (Clean indoor air / clean drinking water) are really just proxies for how clean our bodies are, (both in terms of pathogen exposure but also of pollutants). I wonder what other tools you could include in a "clean body" framework? My first thought was about the potential for blood-donation to filter out bio-accumulated microplastics from the body (reducing the concentration as newly made blood does not contain any), but I'm sure there are other examples.
Great post, looking forward to more!
Ulrik Horn @ 2023-05-08T03:41 (+5)
A couple of thoughts:
-The solar analogy might need to be caveated - solar has been massively deployed because it outcompeted another energy source. Clean air is not in demand and is therefore quite different.
-One way to make people have clean air demand is for them to notice how much better their life becomes after they have clean air. I think there is a better setting for making people realize this than hospitals, offices and even schools: Pre-school. As a parent, kids get sick at an absurd rate in pre-school and it places great stress on the family. Also, it would be super easy to just oneself set up a pre-school with best-in-class air quality in a neighborhood with resourceful parents. These would then spread the word to other parents of how seldom the kids are sick and you can actually create a large business of pre-schools based on having kids that are much less sick.
SiebeRozendal @ 2023-06-01T13:00 (+3)
Love this idea! Visible effects, interested consumers
Ulrik Horn @ 2023-06-02T05:52 (+1)
Desperate consumers - I am talking from first hand experience, haha! I'll get in touch to see if you want to collaborate after my current project is handed over or winds down. That is, unless I find something else to do. Feel free to reach out to me anytime for an update.
Michael_Wiebe @ 2023-05-18T18:51 (+4)
Has anyone thought about the effects of air pollution on animal welfare?
BenSchifman @ 2023-05-02T16:43 (+3)
Great post. I understand indoor air quality is the focus of the piece but if we're looking holistically at clean air we should also consider the significant health costs of air pollution outdoors. Patrick Collison has a great overview: https://patrickcollison.com/pollution
JoshuaBlake @ 2023-06-23T15:22 (+1)
Intesesting article and framing, thank you. I've only just got round to reading it but have a few questions.
First, by clean air, do you mean low CO2 or no pathogens? These seem to have quite different solutions and benefits but the article doesn't cleanly distinguish. Most of the solutions (excepting ventilation) do not reduce CO2 levels, and hence would not give the benefits to cognition etc that ventilation do. Furthermore, monitoring CO2 levels won't tell you much because, once you implement these solutions, the link between CO2 levels and pathogen levels is broken.
Second, I'm not convinced the evidence supports the size of benefit you suggest here: near-elimination of respiratory illness through clean air alone. The updated 1DaySooner report (which I appreciate wasn't published when you wrote this piece) estimates reducing transmission by 30--75%. While the mid-to-top-end of that range might remove flu epidemics (R0 up to around 2) as a threat, this seems less likely for all respiratory illnesses such as endemic coronaviruses (R0 around 10) or even original, Wuhan SARS-CoV-2 (R0 at least 3, likely 4 or higher). It certainly wouldn't be enough for measles (R0 15--20). Indoor air cleaning still seems valuable but I wouldn't want to oversell it as a silver bullet, rather than one line in multi-factorial pathogen defence.
Finally, I was wondering if there was a reason you didn't mention the update to UK building regulations to include indoor air quality (published 2021). These look really promosing to me, although I'm not an expert in either the regulatary or technical side, so would appreciate further commentary!
