Air Safety to Combat Global Catastrophic Biorisks [REVISED]
By G_Klw, Alastair Fraser-Urquhart, joshcmorrison @ 2023-05-03T18:25 (+60)
This is a linkpost to https://drive.google.com/file/d/1QKusCnLzUs041nIuiq6nMxSIRcXaGiKq/view
This report is a collaboration between researchers from 1Day Sooner and Rethink Priorities.
Overview
This post is a revision of a report previously published on how improvements in indoor air quality can address global catastrophic risk from pandemics. After feedback from expert reviewers, we revised the report in accordance with comments. The comments greatly improved the report and we consider the earlier version to be misphrased, misleading, or mathematically underspecified in several places, but we are leaving the post available to illustrate the revision process.
Unlike in the previous post, we are not including the full report, given its length. Instead, this post contains a summary of the reviews and of the report, with a link to the full report.
Many thanks to the expert reviewers (listed below) for their detailed feedback. Additional thanks to Rachel Shu for research and writing assistance. We also received help and feedback from many other people over the course of this process—a full list is in the “Acknowledgements” section of the report.
Summary of Expert Review
We asked biosecurity and indoor air quality experts to review this report: Dr. Richard Bruns of the John Hopkins Center for Health Security, Dr. Jacob Bueno de Mesquita and Dr. Alexandra Johnson of Lawrence Berkeley National Lab, Dr. David Manheim of ALTER, and Professor Shelly Miller of the University of Colorado.
These experts suggested a variety of both minor and substantive changes to the document, though these changes do not alter the overall conclusion of the report that indoor air safety is an important lever for reducing GCBRs and that there are several high-leverage funding opportunities around promoting indoor air quality and specific air cleaning interventions.
The main changes suggested were:
- Providing confidence intervals on key estimates, such as our estimate of the overall impact of IAQ interventions, and reframing certain estimates to improve clarity.
- Modifying the phrasing around the section concerning ‘modelling’, to better clarify our position around the specific limitations of existing models (specifically that there aren’t models that move from the room and building-level transmission to population-level transmission).
- Clarifying the distinction between mechanical interventions, specific in-duct vs upper-room systems (254nm) and HVAC-filtration vs portable air cleaners and adding additional information about some interactions between different intervention types
- Adding general public advocacy for indoor air quality as a funding opportunity and related research that could be done support advocacy efforts.
- Adding additional relevant literature and more minor details regarding indoor air quality across different sections.
- Improving the overall readability of the report, by removing repetitive elements.
Report Executive Summary
Top-line summary
- Most efforts to address indoor air quality (IAQ) do not address airborne pathogen levels, and creating indoor air quality standards that include airborne pathogen levels could meaningfully reduce global catastrophic biorisk from pandemics.
- We estimate that an ideal adoption of indoor air quality interventions, like ventilation, filtration, and ultraviolet germicidal irradiation (GUV) in all public buildings in the US, would reduce overall population transmission of respiratory illnesses by 30-75%, with a median estimate of 52.5%.
- Bottlenecks inhibiting the mass deployment of these technologies include a lack of clear standards, cost of implementation, and difficulty changing regulation/public attitudes.
- The following actions can accelerate deployment and improve IAQ to reduce biorisk:
- Funders can support advocacy efforts, initiatives to reduce cost and manufacturing issues, and research with contributions ranging from $25,000-$200M. Applied research projects can be funded to show the efficacy of ventilation, filtration, and GUV in field applications.
- Businesses and nonprofits can become early adopters of GUV technology by installing it in their offices and allowing effectiveness data to be collected.
- Researchers can develop models that better tie built-environment interventions to population-level effects, conduct further GUV safety testing, and do fundamental materials and manufacturing research for GUV interventions. Applied research can be conducted on ventilation, filtration, and GUV applications in real settings.
The problem: airborne pathogens
Infectious diseases pose a global catastrophic risk. The risk is especially severe, and we are far less prepared, if it involves bioengineered pathogens. Out of the various methods of pathogen transmission, airborne pathogens, particularly viruses, are especially dangerous, as they are easy to spread and difficult to combat. Airborne pathogens are significantly more likely to spread indoors than outdoors, so reducing indoor respiratory pathogen transmission could substantially reduce global catastrophic biorisk by:
- Reducing the probability that a disease has an effective reproduction number >1 and will spread at all, or if not,
- Limiting the number of infections that occur, "flattening the curve" so as not to overwhelm medical systems
- Slowing the spread of disease to
- Provide more time for countermeasure development, and
- Discuss and implement non-pharmaceutical interventions, like limiting large gatherings and requiring masks.
Current indoor air standards do not consider infectious disease risk, whereas waterborne and foodborne pathogen deaths have been largely eliminated in many areas due to improved water and food sanitation. Indoor air quality, especially concerning infectious diseases, should be a priority public good, like fire safety, food safety, and potable water.
How to fix indoor air contamination
Known effective interventions to reduce indoor air pathogen contamination include increased outdoor air ventilation, high-efficiency particulate air (HEPA) filtering, and germicidal ultraviolet (GUV) light. Of these, GUV technology is the most promising for pathogen control because it can reach considerably higher levels of equivalent air changes per hour (eACH) than filtration or ventilation by directly inactivating pathogens, could in principle be more energy efficient, is straightforward to install as a retrofit, and produces no noise pollution. Filtration is a viable option for high levels of eACH up to CDC hospital standards (8-12 eACH), where it is still relatively cost-effective. It also helps to reduce particulate and chemical pollution, which is relevant for immediate health concerns, such as chronic respiratory health and everyday cognitive functioning. By contrast, high-volume ventilation is expensive, or even impossible in many buildings due to the difficulty of retrofitting or upgrading HVAC systems.
Currently, two different wavelengths of GUV are utilized: 254 nm UVC and 222 nm UVC, also known as far-UVC. People should not be directly exposed to 254 nm UVC, since it can cause skin and eye damage, but 222 nm UVC is likely safe for direct interaction. Most current germicidal light fixtures are 254 nm, and therefore installed as an upper-room or in-duct system, shielded from room occupants.
- 254 nm UVC is already more cost-effective than other IAQ interventions and, if installed correctly, is safe due to lack of interaction with a room’s occupants.
- Far-UVC can be used to reduce surface and close contact transmission as well as airborne transmission, making it potentially the most effective intervention for reducing global catastrophic biorisk, with a recent review indicating strong safety evidence in humans even after prolonged exposure. The price of current systems is currently too high for at-scale deployment, though there are reasons to think the price can be lowered significantly.
We estimate that the ideal mass deployment of indoor air quality interventions, like ventilation, filtration, and GUV, would reduce overall population transmission of respiratory illnesses by 30-75%, with a median estimate of 52.5%. (Described in the “Rough estimate of impact” section.) This could completely prevent many current diseases from spreading, and even for the most transmissible diseases, like measles, it likely amounts to a great reduction in transmission speed, and would serve as an important layer of biodefense.
Overall, we can be confident that these interventions effectively reduce pathogen load in the air, and some previous work has been done investigating the impact of ventilation on population-level transmission.
How can we accelerate the deployment of IAQ-related interventions?
Despite the existence of promising technologies, several bottlenecks are preventing the mass deployment of IAQ interventions. Some significant ones include:
- Expense of improving and implementing air cleaning technology.
- Difficulty of wide-scale change in regulations and public attitudes towards indoor air quality.
- Difficulty in understanding the relationship between pathogen load and infection cases.
However, significant opportunities exist to accelerate deployment via advocacy, cost and manufacturing improvements, and research.
- Advocacy: Some presently attractive advocacy projects include: development of an anti-infection standard by the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE); promoting use of the recently released (Non-infectious Air Delivery Rate) NADR standard from the Lancet COVID Commission; recruiting high-status businesses as early adopters who can conduct and fund pilots; improving air quality in schools through private and public investments; and creating an umbrella group to coordinate efforts.
- Costs and manufacturing: Advanced market commitments and other forms of investment could drive down the cost of far-UVC solid-state emitters and other interventions. Investments in training could also increase expertise in design and installation of GUV systems.
- Research: Attractive research opportunities include: (a) further establishing the long-term safety of far-UVC, which can help with international deployment, (b) creating reliable ways to test intervention efficacy, which could include applied research programs or controlled natural exposure challenge studies, (c) developing guides to help organizations optimally deploy IAQ fixtures, and (d) social research to improve public advocacy efforts around IAQ.
We provide a conservative estimate that the total cost of upgrading air quality systems in all public buildings in the US to be $120-$420 billion (CI:90%).
We give a conservative estimate that reducing the risk of a future pandemic as bad as COVID by 1% would be worth $100 billion, and it seems highly likely that this program would reduce the risk or severity of a pandemic by more than 1%.
We think significant action to accelerate deployment of IAQ interventions to reduce biorisk would benefit from philanthropic funding in the range of $25,000-200M:
- $25,000 could fund the development of a detailed population transmission model or message-testing surveys for IAQ public advocacy.
- $5M could fund the development of new solid-state far-UVC light sources.
- $20M could fund a single dedicated clinical project (e.g., something like EMIT-2) or a field demonstration of GUV efficacy in reducing transmission in high risk areas.
- $200M could fund a program combining studies to ascertain and demonstrate the effect of indoor air interventions with advocacy to lead to broad adoption (e.g., far-UVC light safety studies, real-world efficacy studies for IAQ interventions, advocacy for improved pandemic preparedness standards, etc.).
Max Görlitz @ 2023-05-04T08:10 (+6)
Thanks for your transparency and for updating this report; I think it is tremendously valuable. I have only skimmed so far, but I will hopefully read through it completely soon.
I also tried to do a back-of-the-envelope calculation of the cost-effectiveness of 254 nm upper-room GUV per eACH a while ago. I estimated higher numbers in my model, more on the order of $100/eACH/year (For context: the report estimates ~$14/eACH/year). Note that the model is pretty rough, but I'll post it anyway in case it proves useful for others.
I think this difference comes mainly from having a much lower point estimate of eACH that is realistically achievable. In general, I am rather skeptical of eACH estimates for GUV that go into the hundreds.
As far as I understand, the way eACH are calculated depends on the specific pathogen in question. Pathogens vary widely in their susceptibility to GUV, and coronaviruses are unusually susceptible IIRC. Since many of these eACH estimates were calculated based on measurements with coronaviruses, this inflates the values, and they'd presumably be significantly lower for other pathogens.
Another point is that AFAICT, the higher eACH estimates mostly (all?) come from computational models and not real-world measurements. I assume that real-world environments are messy and will be less ideal for achieving very high eACH rates.
I think I had another reason for my skepticism, but unfortunately, I can't recall it right now—will update this comment should I remember.
Gavriel Kleinwaks @ 2023-05-09T17:05 (+1)
Thanks so much for the kind feedback and comparison calculation! Your skepticism about the eACH estimates is warranted--I was unaware that coronaviruses were unusually susceptible (compared with other viruses, you mean?); the estimates we saw were all based on either SARS-CoV-2 or tuberculosis (also quite susceptible). It's useful to know how other people are approaching this question, and ultimately the problem calls for much more extensive real-world observations.
Max Görlitz @ 2023-05-09T18:25 (+1)
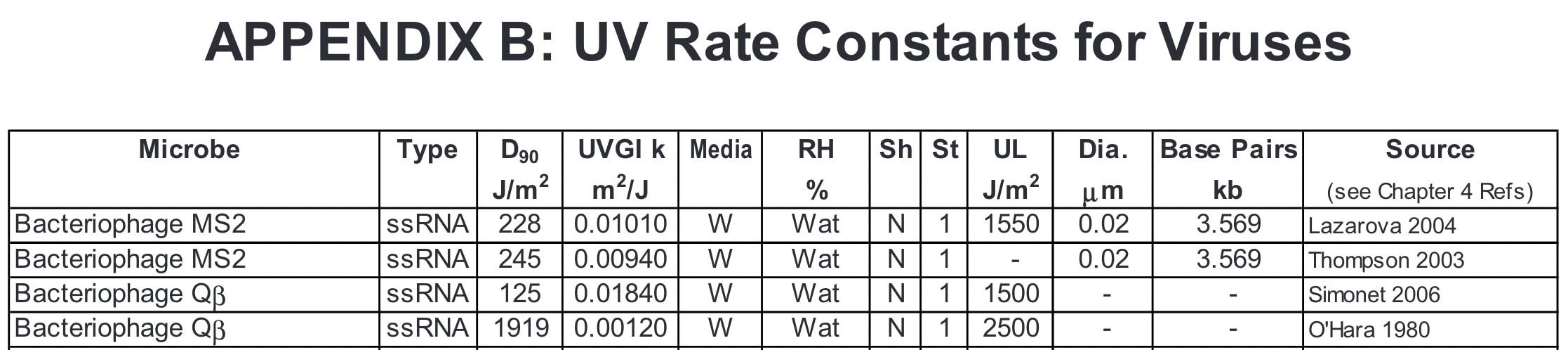
Yea, the way I recall it is that coronaviruses are more susceptible than other viruses. I first tried to recheck this in Appendix B of Kowalski (2009), but the values provided there vary extremely widely. I suspect the experimental quality varies a lot between those estimates, and coronaviruses were, of course, of much less interest back then.
[...]
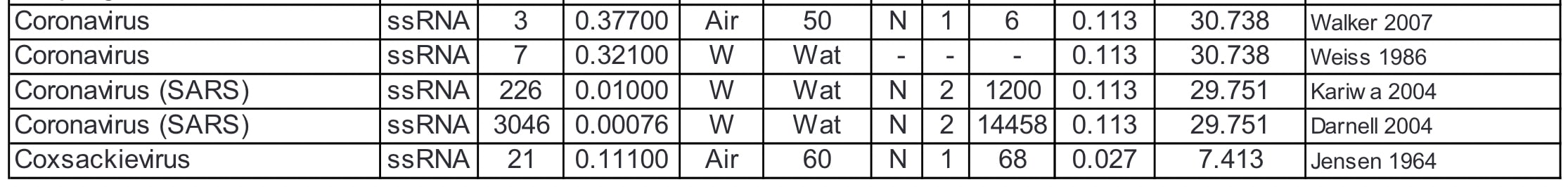
IMO, the easiest way to read these values is the D90 (J/m^2) value, the dose required to inactivate 90% of viruses in a sample. This is equivalent to speaking about a "1 log reduction".
Blatchley et al. (2022) have more recent data and provide better evidence for coronaviruses being especially susceptible:
"At 254 nm approximately 1 log10 reduction of coronaviruses is achieved for each 2 mJ/cm2 delivered UV-C fluence (dose). For comparison, other human pathogenic viruses, such as poliovirus and rotavirus require about 4–5 times that amount (i.e., 8–10 mJ/cm2) for each log10 unit reduction (Masjoudi et al., Citation2021).
UV222 irradiation is at least as effective as UV254 irradiation for inactivation of viruses, with approximately 1 log10 reduction of coronaviruses achieved for each 1 mJ/cm2 of delivered UV-C fluence or less. In other words, irradiation at 222 nm provides roughly twice the rate of inactivation as observed at 254 nm."
On the other hand, when considering catastrophic biorisk, we mostly don't care about, e.g., poliovirus, but other viruses with more pandemic potential, such as Influenza. So the more productive comparison could be restricted to these high-profile pathogens. I haven't taken the time to compare all their UV susceptibility values. If they turn out to be similar to those of coronaviruses, my skepticism of high eACH estimates might not be as valid.