Cause Exploration Prizes: Time-restricted eating (IF) for individual and community health in LMICs
By Coefficient Giving @ 2022-07-12T07:26 (+8)
This anonymous essay was submitted to Open Philanthropy's Cause Exploration Prizes contest and posted to the Forum with the author's permission.
This Cause Exploration Prizes submission is organized into the following sections:
- Discussion of the opportunity to expand the practice of time-restricted eating — i.e., intermittent fasting (IF) or caloric restriction — for human health: with expected material co-benefits for economic welfare in LMIC markets, and expected non-zero benefits for animal welfare, climate change, mental health, and food-related violence prevention
- An Importance, Tractability, and Neglectedness evaluation of this cause area
- Example grants that could be made (e.g., to Development Media International, academic institutions, and Innovations for Poverty Action) in this cause area
- Outstanding questions to investigate for this cause area
- Concluding note
- Attachments
DISCUSSION
Major news organizations and leading academic institutions — Cleveland Clinic, Harvard Medical School, and Johns Hopkins University among them — have noted a “growing body of research” that shows time-restricted eating can serve as “a realistic, sustainable, and effective approach for weight loss, as well as for diabetes prevention.”[1] This approach is also known as intermittent fasting (IF). Prominent medical school faculty at Harvard and Yale; business leaders like Jack Dorsey; musicians like Moby; actors like Jennifer Aniston, Halle Berry, Hugh Jackman, and Chris Pratt; and celebrities like Gisele Bündchen and Jimmy Kimmel are among IF followers.[2] At least one Harvard Medical School professor — a leader in the American College of Cardiology — has also suggested that more patients of Asian heritage explore IF as to achieve cardiovascular and cancer health benefits.[3]
Time-restricted eating appears to be a niche, if growing, practice in obesity-burdened OECD countries. Credible leaders in academic medicine, business, and the entertainment and self-improvement industries[4] are helping to popularize IF among a subset of information-rich consumers. At the same time, researchers are finding that traditional Western diets and influences are a factor in growing obesity-related problems in LMICs. An example is Nigeria, where The Guardian in 2014 noted “that western influences on diet and lifestyle are playing a part in what looks set to be a serious epidemic”:
Weight goes with wealth in Nigeria today. The richest women are three and a half times more likely to be overweight or obese than those in the lowest income bracket. That is not so surprising. But education and social status also increase women's chances of putting on more weight than is good for their health. In Nigeria, there is a cultural element to this - richer and more successful women are expected to be fatter. But part of this is the pursuit of a lifestyle that is presumed to be enviable because it is that of people in the affluent nations of the world like the US and the UK. They emulate our success and are landed with our problems.
The negative externalities of Western-style overeating are only mounting in the 2020s. A pandemic and a land war in Eastern Europe’s breadbasket have sent global competition and prices for food staples to all-time highs. At the same time, over the last decade effective funders have made several promising grants to nonprofits that look to improve individual and community health by communicating best practices in LMICs. Development Media International (DMI) received funding from GiveWell and Open Philanthropy for “radio and television programming in developing countries that encourage people to adopt improved health practices,” including mass-media campaigns to promote COVID-19 NPIs.
Cost-effective[5] campaigns to educate LMIC households about healthy IF practices would be expected to influence a small share of individuals, but still generate benefits in terms of:
- Individual health: expressed in QALYs obtained via better outcomes for cancer patients and some individuals with diabetes or prediabetes, and other health benefits
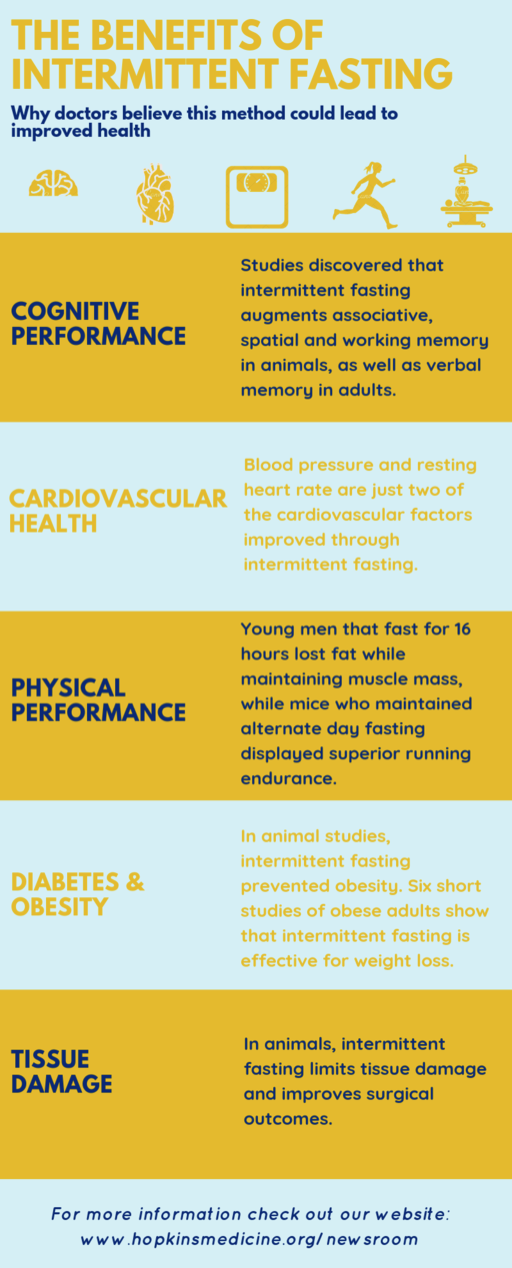
- See The Benefits of Intermittent Fasting sidebar from Johns Hopkins Medicine on page 4 of this memo, which summarizes benefits to cardiovascular health, cognitive performance, and other endpoints associated with IF
- Economic returns to households and communities/nations: popular IF plans, such as the 5:2 approach, result in fewer weekly calories eaten overall. IF practitioners have noted the personal financial benefits of spending less on food while achieving better health outcomes, cost savings that should be even more salient in LMIC contexts. Even if a very small percentage of households in food-insecure countries such as Nigeria safely and healthily trim their food consumption, the result should be marginally more supply and fewer shortages. IF-practicing individuals should enjoy more disposable income versus those following standard Western diets, and their countrymen would be expected to enjoy slightly more food availability
- The positive externalities of reducing overeating and localized food shortages could include: fewer lost labor days due to improved workforce health over time, marginally less strain on healthcare resources driven by diseases of obesity (or hunger), reallocation of “excessive food expenditure” to higher- value uses, and less violent unrest related to food price and supply shocks
- Co-benefits for other important, tractable, and neglected causes, such as:
- Reducing farm animal suffering: a reduction in excess calorie demand should reduce aggregate food demand, including demand for animal products. (Time-restricted eaters may also become more attentive to their diets generally, and perhaps explore plant-based diets as a way to improve health)
- Trimming carbon emissions associated with localized oversupply of calories to households and individuals: similarly, trimming aggregate calorie demand would be expected (over time) to lead to an infinitesimally slower growth rate in the food sector. Since food systems account for over ⅓ of global GHG emissions, however, even tiny changes to the sector’s growth rate would be expected have non-zero impact on a country’s greenhouse gas emissions
- Reducing the mental health burden for some individuals on calorie-restricted diets out of economic necessity: by enabling them to experience the cognitive benefits of an IF diet, versus an equally low-calorie, less well-structured diet — and perhaps by rebranding caloric restriction diets as “the smart diet of healthy, cosmopolitan millionaires” [such as those in Appendix D] as opposed to the stigmatized last resort of the poor and food-insecure
Without drafting detailed BOTECs for each of these categories of social benefits, my sense is Category 1 is around an order of magnitude more important than Category 2 — which in turn may be an order of magnitude more important than all expected benefits from Category 3.
IMPORTANCE, TRACTABILITY, AND NEGLECTEDNESS EVALUATION
Importance: in December 2019, the World Health Organization noted that “almost 2.3 billion children and adults are overweight, and more than 150 million children are stunted” — as many LMICs experience “both extremes of malnutrition,” hunger and obesity.
- IF is not advised for children. Assuming more than 1 billion of the world’s overweight adults are in China, OECD countries, or other nations less-suited for affordable and flexible mass-communication campaigns, a rough estimate could be that 500 million overweight adults in South Asia, Southeast Asia, and sub-Saharan Africa are potentially reachable via IF education campaigns
- A 2020 paper on life expectancy for obese, overweight, and healthy weight Ghanaians estimated that overweight Ghanaians (of either gender) lived about two fewer years than healthy weight Ghanaians, and that obese Ghanaian women died more than two years earlier than overweight women - while obese Ghanain men died more than three years earlier than overweight men
- IF is not a fail-proof “silver bullet” for obesity-related health impacts. That said, considering the Ghanaian data, it is conceivable that well-designed, wide-ranging campaigns in LMICs could lead hundreds of thousands of adults to enjoy additional months of healthspan and lifespan (on average) due to IF-associated cardiovascular, renal, and other health benefits. In expectation, this would lead to longer working lives, lower chronic disease burdens for families and societies, and economic benefits from better capital allocation: away from low-value food spending, and avoidable chronic and serious disease-related costs
Tractability: I confess that I have very little confidence in my ability to estimate the impact per dollar for different types of IF-related interventions. That said, I expect that effective funders — perhaps working with other funders focused on noncommunicable diseases, such as Michael Bloomberg and his organizations — could work with nonprofits like DMI, Innovations for Poverty Action, and other credible organizations on pilot projects in one or more LMICs to better gauge the ROI of interventions in this cause area.
Neglectedness: aside from scattered IF articles in the Indian and South African popular press (or in sites serving diabetes patients), it seems that IF is rarely studied as an intervention in LMICs. For example, the Google Searches “intermittent fasting” +LMICs and “caloric restriction” + LMICs generate zero relevant search results. Two possible explanations are:
A. This is another case, among many, in the delayed arrival of cutting-edge health research and best practices in LMICs
B. This problem is less tractable and/or less important than I realize, and has been deprioritized as a cause for sensible reasons
At this point I have 65% confidence that explanation A. is the more-important factor leading to the research gap in this cause area. IF is seen as an eccentric and/or daunting practice among many in OECD countries, where it is better-known — the growing scientific consensus in IF’s favor aside. However, explanation B. remains a very real possibility.
SAMPLE GRANTS THAT COULD BE MADE IN THIS CAUSE AREA
For “hypothetical grantee” diversity, I'm including three sample grants here — to A) a major university, B) a non-profit research organization, and C) DMI, as a direct actor in LMIC public health media.
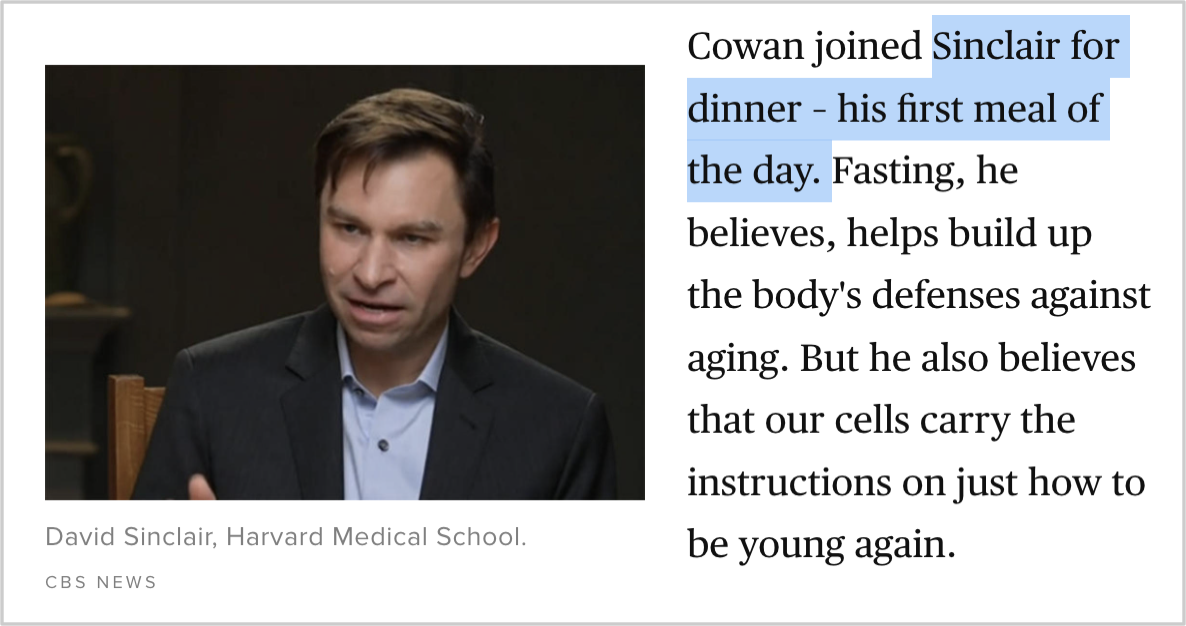
- I would explore a grant to relevant teams at Harvard’s T.H. Chan School for Public Health, perhaps to include the school’s India Research Center. Harvard Medical School’s publishing arm, Harvard Health, has long advocated for its readers to consider practicing IF. HMS’s David Sinclair is also one of IF’s most-prominent boosters. A multi-year RCT could explore how communications campaigns amplifying Harvard’s recommendations around IF’s benefits affect low-income Indians’ propensity to experiment with time-restricted eating. If the advertising campaigns are found to drive behavior change, the study could evaluate if new IF adherents report health and/or economic benefits from the practice
- A grant to Innovations for Poverty Action could support IPA’s efforts to evaluate the effectiveness of an IF campaign in South Asia, Southeast Asia, or Sub-Saharan Africa. IPA has been engaged in independent verification of the work of DMI in the past, and could be well-placed to design/verify any pilots related to this cause area
- GiveWell’s mid-2010s assessment of Development Media International as unusual in its commitment to self-analysis and transparency could make it a strong partner for a pilot communications project on IF. DMI’s ability to broadcast pandemic-relevant public health information in nine African countries during 2020 also suggest it is well-placed to experiment with interventions in one or more states, if cultural or economic differences could lead to strong regional variation in the effectiveness of IF-driven public health campaigns. (I suspect there are, but am not familiar with, nonprofits with DMI-style approaches to broadcasting, transparency, and rigorous self-analysis in South Asia and Southeast Asia. These could also be grantees)
- DMI’s 2020-2021 annual report notes that “a survey we commissioned in Burkina Faso showed an extraordinary 81% of women cited radio as their primary source of information about COVID-19 (followed by friends at 6% and health facility staff at 3%).” If those figures are directionally accurate, radio in Burkina Faso could be a powerful channel for helping Burkinabé households adopt caloric restriction practices that have been found to enhance cognitive and physical health — as opposed to less-structured caloric restriction, which offers far fewer health benefits due to the lack of hormesis
OUTSTANDING QUESTIONS FOR THIS CAUSE AREA
Major outstanding questions for this cause area include:
- What are BOTECs in terms of the expected costs versus expected benefits for caloric restriction/IF education-related projects in different LMICs?
- DMI reported that they achieved 15 million views on social media and reached 141 million people in their 2020-2021 reporting period, a year in which they spent £8.4 million. How many of those views are attributable to new content published in that reporting year (versus legacy content that DMI paid to publish in the 2010s, for example) is less clear. DMI’s realized cost-per-impression likely varied meaningfully across the nine countries, 81 languages, and 412 radio stations with which DMI worked
- For example, the World Bank reports that per-capita GDP (in current USD) in Côte d'Ivoire is roughly five times that of per-capita GDP in Madagascar and Mozambique, and nearly triple that of per-capita GDP in Burkina Faso. Since DMI works in all four countries, and media consumption and production costs vary between and within states, one could expect significantly different “fully loaded” costs of impression by market
- Similarly, the availability and price of food — and the incidence of hunger, obesity, food-related violence and social unrest, and other ills — will vary across LMIC communities. So too will cultural receptivity to advice about caloric restriction and a potentially faddish-seeming eating practice popular among some wealthy Americans and Europeans. I do not yet have a strong ex ante view as to which LMIC regions would see the greatest returns from exposure to healthy caloric restriction practices, or how the “benefit” side of a cost-benefit analysis BOTEC would turn out in Bihar versus Burkina Faso
- Can a well-designed, well-meaning, and high-impact education campaign about IF and time-restricted eating be insulated against (perhaps equally well-intentioned, if counterproductive) anti-colonial critiques? An ungenerous but accurate description of a campaign like this might be: “Affluent Westerners are telling the poorest countries in the world how they should eat less during a worldwide food crisis. [Perhaps they should instead focus on cutting food waste on their own turf, and eschew luxury spending to help feed those in food-insecure regions?]”
- Strategies to reduce this risk could include:
- Investing in culturally competent communications, including by highlighting credible validators (e.g., these “Intermittent Fasting for South Asians” presenters, who are physicians of South Asian descent) for healthy caloric restriction. Dr. Ami Bhatt of the American College of Cardiology and Harvard Medical School, referenced in Appendix B, is also passionate about health equity and the promise of IF. Key opinion leaders like Dr. Bhatt could serve as essential advocates
- Framing savvy caloric restriction as an aspirational practice used by energetic billionaires and millionaires — such as those in Appendix D — rather than a cold, dietary austerity for thee, but not for me-style campaign designed by self-serving/neocolonial Western interests. Healthy caloric restriction can also be framed as an opportunity for LMIC communities to “leapfrog” the most harmful effects of obesity and the Western diet, without experiencing the same costly explosion of cardiovascular and kidney health issues (along with premature death and disability) that many OECD countries are experiencing
- Strategies to reduce this risk could include:
- Are there “grasstops”-focused strategies that would help healthy IF and caloric restriction to achieve viral adoption in certain communities — as a successful meme, rather than the counterproductive, neocolonial-seeming meme risk described in question 2?
- Healthy and successful IF devotees (such as those in Appendix C and D) have served as important validators for the practice in Western societies. Beyond broadcast promotion via DMI-style radio and mobile video channels, another approach could be to cultivate trusted regional validators among celebrities, athletes, respected academics, star physicians, and others
- Hollywood stars have led healthy IF practices to earn coverage in Marie Claire, People and Us magazines. Bollywood and Nollywood stars could serve as powerful ambassadors for healthy fasting practices in Asia and Africa, especially if there are cultural cross-currents in Nigeria or elsewhere that may frame Western-style excess eating as a prosperous, worldly diet. Cosmopolitan celebrities and top physicians could provide a valuable counter-narrative to the problem highlighted by The Guardian on page 1
ATTACHMENTS
Appendix A: These pages include illustrated transcript excerpts from a national CBS News segment (YouTube link) featuring Dr. Morgan Levine of the Yale School of Medicine; Dr. David Sinclair of Harvard Medical School; and other medical experts who practice IF themselves or have otherwise studied the benefits of caloric restriction and time-restricted eating.
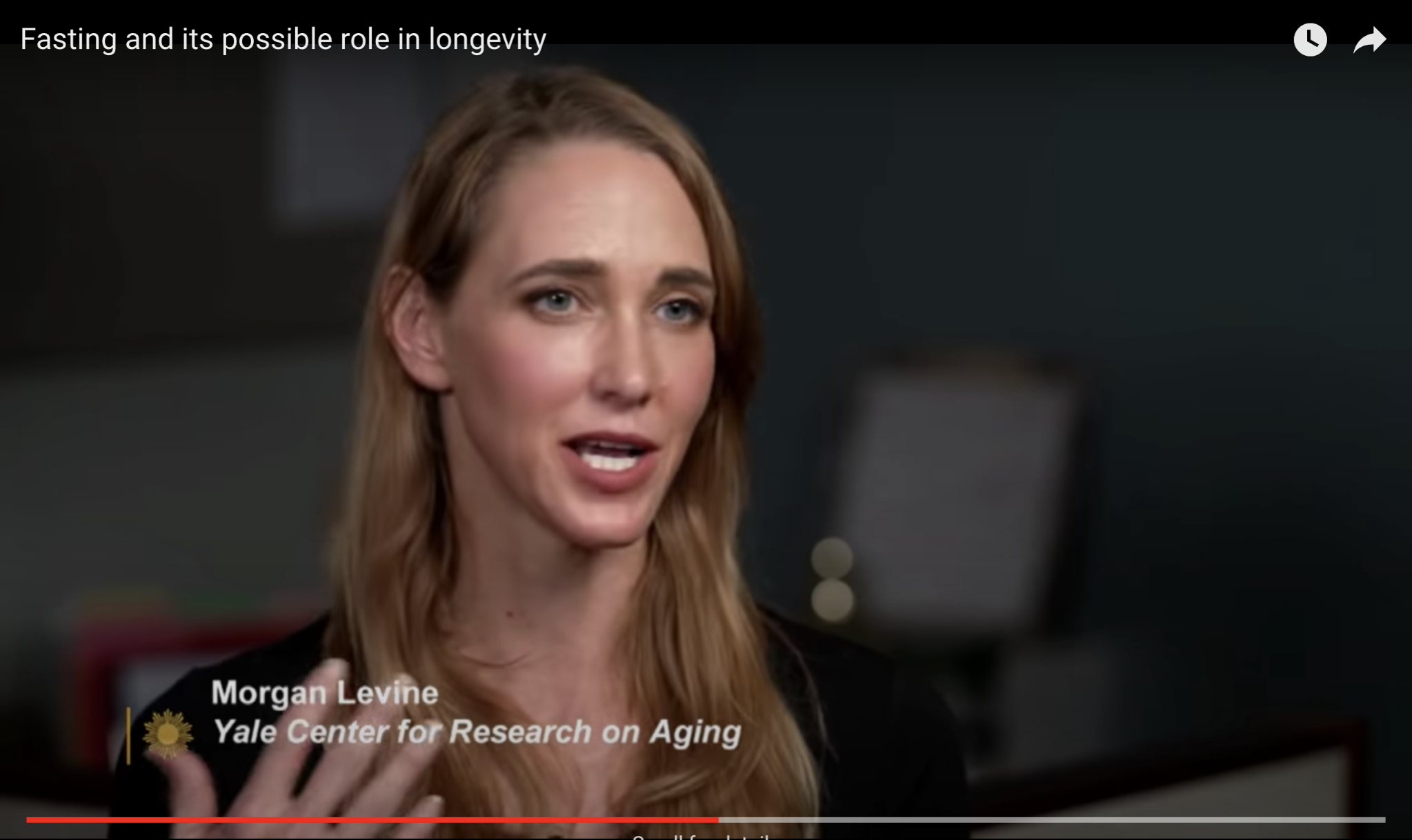
CBS News Transcript —
Dr. Levine (Yale School of Medicine): When your body undergoes a very mild stressor, we’re not talking about a major stressor, it actually becomes a little more resilient. So it’s kind of this: “what doesn’t kill you makes you stronger.” So these really acute mild stressors actually can boost the resilience of your biology, and we think that things like fasting, or caloric restriction, is actually acting through that. And also the same thing as exercise: exercise is actually a stressor on the body, but we think it’s actually the body’s response to this — this is what gives it the benefit.
Interviewer: You’ve been doing this now for a long time. What do you do personally?
Dr. Levine: I eat a plant-based diet, and I try to do what’s called intermittent fasting. Again: the science is still out on whether this is having a big impact. I try to restrict the time I eat during the day to about six hours, and then fast the rest of the day. I usually eat my first meal atone in the afternoon, so around lunchtime, but maybe a little later lunch, and then I try and make sure I don’t eat anything past 8pm. So, I basically brush my teeth when my daughter’s going to bed, and that’s it.
Interviewer: So is this your first meal of the day? It’s now, almost six o’clock.
Dr. Sinclair (Harvard Medical School): It will be, yeah.
Interviewer: No breakfast, no lunch? [No.] Because?
Dr. Sinclair: Well, because it’s clear, based on thousands of years of human existence, that eating less — if it’s not starvation or malnutrition — it’s good for you.
Interviewer: Because why?
Dr. Sinclair: Well, so we didn’t know why it was good for you. We thought it was slowing down metabolism. But it’s not the case… if you choose not to eat a meal or two, you’re turning on the body’s defenses against aging.
Dr. Nir Barzilai (Albert Einstein College of Medicine): People assume that [eating less for health] means you give less [food] for breakfast, lunch, and dinner.
Interviewer: You just eat less throughout the day… but that’s not what it is, though, right?
Dr. Nir Barzilai (Albert Einstein College of Medicine): No. If we actually are giving them all the food throughout the day, they are thinner but they don’t live longer. So you need the fasting to operate your latent mechanism for aging.
Appendix B: LinkedIn post discussion between Harvard Medical School’s and Massachusetts General Hospital’s Ami Bhatt, MD, FACC, the chief innovation officer of the American College of Cardiology, and Jennifer Joe, MD, about the benefits of IF for patients of Asian descent. (Note: I have met both Dr. Bhatt and Dr. Joe in the context of my role as a senior director at Mayo Clinic, and know they are respected in their fields, but am submitting this idea in a purely personal capacity.)
Appendix C: A list of actors, business leaders, and celebrities who may contribute (usefully) to the perception that caloric restriction and IF are signs of sophistication and “smart diets,” rather than stigmatized practices for those unable to afford three meals a day.
- Jennifer Aniston: “‘I do intermittent fasting, so there's no food in the morning,’ [Aniston] told Radio Times... ‘I noticed a big difference in going without solid food for 16 hours.’…The star fasts every day and reserves Sundays as her ‘cheat day.’”
- Halle Berry: “One of a number of celebrities who do intermittent fasting, Berry has found great success with the time-restricted style of eating…. ‘I normally eat two meals a day,’ Berry said in an Instagram story in August 2018, going on to say that she would ‘normally skip breakfast’ and ‘sort of fast’.”
- Jack Dorsey: “The Twitter CEO revealed that he eats only one meal per day: ‘Just dinner,’ he said during a Q&A with fans in a video for Wired…he eats once at dinnertime, between the hours of 6:30 and 9 p.m… ‘During the day, I feel so much more focused,’ he said on the podcast of his fasting.”
- Jimmy Kimmel: “Kimmel explained that people have called his particular method the 5:2 diet - when five days a week are normal eating days, while the other two days you can only consume 500 to 600 calories a day, according to Healthline - but he's been following the same structure since before it had a name linked to intermittent fasting.
- Gisele Bündchen: “In her book Lessons, Bündchen revealed she follows the popular 5:2 version of intermittent fasting, which involves eating normally on five days of the week and restricting calories to 500-600 calories on the remaining two. While the fasting window is up to the individual, the Brazilian supermodel explained she fasts until lunchtime two days of the week to allow her body time to rest and digest.”
- Moby: “‘I actually do intermittent fasting every day," the singer told Us in October 2018. ‘I try minimum 12 hours, usually 16. Basically, I just don't eat dinner.’”
- Hugh Jackman: “[Jackman] has often relied on an intermittent-fasting plan to drop the weight he’s required to put on for action-movie roles. ‘I feel so much better on it,’ he said. ‘I haven’t put on nearly the amount of fat I normally would. And the great thing about this diet is, I sleep so much better.’”
- Kourtney Kardashian: “‘I wouldn't eat past 7 p.m. at night and then I would wait to eat the next day until after my morning workout, which would be around 10:30 a.m. or 11 a.m.,’ she said. ‘Then, one day a week, I did a 24-hour fast.’”
- Chris Pratt: “‘So I'm doing this intermittent fasting thing; don't eat till noon, try to get my cardio in in the morning. It's super exciting actor stuff,’ Pratt joked on Instagram. …Pratt encouraged his followers to read up on intermittent fasting after his quick success. ‘Look it up! Check it out! It's actually kinda cool,’ he continued. ‘Works pretty good and I've lost a little weight so far.’”
Appendix D: A final example of a wealthy, high-status practitioner of intermittent fasting is the New York Times-bestselling author James Clear (~698K Twitter followers). Per Amazon, his self-help book Atomic Habits has “sold over 5 million copies worldwide and has been translated into more than 50 languages.”
Note — James Clear himself has resisted caloric restriction within IF. As a former college athlete he regularly lifts weights and tries to “maintain weight,” but he has also written:
[M]ost people who try intermittent fasting end up losing some weight because the size of their meals remains similar even though a few meals are being cut out each week. If you're looking to lose weight, this isn't a problem.
- ^
“Intermittent fasting: The positive news continues,” Harvard Health, Harvard Medical School, https://www.health.harvard.edu/blog/intermittent-fasting-surprising-update-2018062914156
- ^
See the national CBS News report in Appendix A for HMS and Yale Med faculty who practice IF, and Appendices C and D for quotes from celebrity practitioners and advocates for time-restricted eating
- ^
See the post from Ami B. Bhatt, MD, FACC, in Appendix B
- ^
Appendix D describes a prominent self-improvement writer’s decade-long advocacy for IF
- ^
These campaigns are expected to generate greater social ROI in LMICs than in wealthier countries, both due to the lower costs of media impressions, and the greater marginal social value of “money redirected elsewhere via avoided costs from overeating-driven healthcare costs and excess spending for food”
Julia_Wise @ 2023-05-12T18:03 (+4)
You note that it's not recommended for children. Seems worth noting there's some (but not good-quality) evidence that fasting isn't a good idea during pregnancy. Review of health outcomes from Ramadan fasting during pregnancy
david_reinstein @ 2022-07-12T11:18 (+2)
Interesting idea but pitching it could be challenging. How to get the messaging right. I can see the headline “celebrities to Nigerians: ‘let them (not) eat cake’ before noon”