AI Mental Health Chatbots for Low-Resource Settings: A Prioritization Framework
By Dawn Drescher, Anand Jeevanandham, Angie Hsu, Scott Blain @ 2025-12-01T17:41 (+10)
Summary: We're building an AI-powered mental health chatbot targeting populations with severe mental healthcare shortages. This post presents our framework for prioritizing which conditions and regions to focus on first, synthesizing data on global mental health workforce gaps, existing digital resources across 15+ diagnostic categories, and AI intervention suitability. A key consideration is “breaking the cycle of trauma and tyranny” – addressing conditions that contribute to insecure attachment and power-seeking behavior that perpetuate conflict and authoritarianism.
Note: This is the summary of our preliminary findings including personal observations and inferences. We consider this level of certainty sufficient for current purposes in this early exploratory phase. We’ve written this article with the assistance of Claude and Gemini. We seek further advice and suggestions for the refinement or reframing of the project’s scope.
Introduction
 The supply of mental health workers per 100,000 population ranges from 67 in high-income countries to 1 in low-income countries. In all settings, though, there are people whose mental health problems are not addressed for lack of affordable and accessible care.
The supply of mental health workers per 100,000 population ranges from 67 in high-income countries to 1 in low-income countries. In all settings, though, there are people whose mental health problems are not addressed for lack of affordable and accessible care.
Recent advances in large language models (LLMs) present an opportunity to partially address this gap through scalable, low-cost interventions. Our team is developing an AI mental health chatbot and hopes to make it useful for populations with the least access to traditional mental healthcare.
However, mental health is vast: various diagnostic manuals contain hundreds of diagnoses each, which overlap in complex ways, and mental health needs vary dramatically across cultural contexts. We cannot effectively serve everyone simultaneously. This post outlines our systematic approach to prioritization and solicits feedback on our reasoning and potential blind spots.
Our Context and Constraints
Team composition: Multilingual team with fluency in English, German, Hindi, Tamil, Estonian, Finnish, and Mandarin.
Unique advantage: Team lead has direct connections within communities struggling with Cluster B personality disorders (ASPD, BPD, HPD, NPD) and familiarity with mentalization-based treatment (MBT), potentially enabling culturally competent outreach to highly stigmatized populations typically underserved by existing resources. Our team also includes licensed psychologists and published psychology researchers.
Long-term motivation: Interest in “breaking the cycle of trauma and tyranny” – addressing the intergenerational transmission of trauma, insecure attachment, and personality pathology that contributes to authoritarian leadership and societal instability. This framework also suggests that healing trauma and fostering secure attachment in this generation can reduce power-seeking pathology and conflict risk in the next.
Current stage: Pre-launch prioritization phase. We’re determining which conditions and populations to serve first, rather than attempting a one-size-fits-all approach.
Methodology: Systematic Resource Mapping
Before prioritizing, we conducted a comprehensive landscape analysis across 15+ major diagnostic categories, examining:
- Existing self-help resources (workbooks, apps, online communities) for each specific disorder
- Evidence-based interventions and their amenability to AI delivery
- Global mental health workforce distribution using WHO data
- Technology adoption patterns and infrastructure constraints
- Cultural considerations affecting mental health help-seeking
- Intergenerational impact on attachment security and power-seeking behavior
Our analysis covered:
- Mood disorders (depression, bipolar I, bipolar II, cyclothymic disorder, dysthymia/persistent depressive disorder, disruptive mood dysregulation disorder, premenstrual dysphoric disorder)
- Anxiety disorders (generalized anxiety disorder/GAD, panic disorder, agoraphobia, social anxiety disorder/social phobia, specific phobias, separation anxiety disorder, selective mutism)
- Trauma and stressor-related disorders (PTSD, complex PTSD, acute stress disorder, adjustment disorders, reactive attachment disorder, disinhibited social engagement disorder)
- Obsessive-compulsive and related disorders (OCD, body dysmorphic disorder, hoarding disorder, trichotillomania/hair-pulling disorder, excoriation/skin-picking disorder)
- Personality disorders (Cluster A: paranoid, schizoid, schizotypal; Cluster B: antisocial/ASPD, borderline/BPD, histrionic/HPD, narcissistic/NPD; Cluster C: avoidant, dependent, obsessive-compulsive)
- Psychotic disorders (schizophrenia, schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, delusional disorder, psychotic depression, substance-induced psychotic disorder)
- Neurodevelopmental disorders (ADHD, autism spectrum disorder/ASD, intellectual disabilities, communication disorders including speech sound disorder and childhood-onset fluency disorder/stuttering, specific learning disorders including dyslexia, dyscalculia, and dysgraphia, motor disorders including developmental coordination disorder/dyspraxia, tic disorders including Tourette syndrome)
- Substance use disorders (alcohol use disorder, opioid use disorder, cannabis use disorder, stimulant use disorder including cocaine and amphetamines, sedative/hypnotic/anxiolytic use disorder, tobacco use disorder, hallucinogen use disorder, inhalant use disorder, gambling disorder)
- Feeding and eating disorders (anorexia nervosa, bulimia nervosa, binge eating disorder, avoidant/restrictive food intake disorder/ARFID, pica, rumination disorder)
- Sleep-wake disorders (insomnia disorder, hypersomnolence disorder, narcolepsy, obstructive sleep apnea, central sleep apnea, sleep-related hypoventilation, circadian rhythm sleep-wake disorders, non-rapid eye movement sleep arousal disorders including sleepwalking and sleep terrors, nightmare disorder, rapid eye movement sleep behavior disorder, restless legs syndrome)
- Somatic symptom and related disorders (somatic symptom disorder, illness anxiety disorder/hypochondriasis, conversion disorder/functional neurological symptom disorder, factitious disorder, psychological factors affecting other medical conditions)
- Dissociative disorders (dissociative identity disorder/DID, dissociative amnesia, depersonalization/derealization disorder, other specified dissociative disorder/OSDD)
- Sexual disorders
- Sexual dysfunctions (erectile disorder, female sexual interest/arousal disorder, male hypoactive sexual desire disorder, female orgasmic disorder, delayed ejaculation, premature/early ejaculation, genito-pelvic pain/penetration disorder)
- Paraphilic disorders (voyeuristic disorder, exhibitionistic disorder, frotteuristic disorder, sexual masochism disorder, sexual sadism disorder, pedophilic disorder, fetishistic disorder, transvestic disorder)
- Disruptive, impulse-control, and conduct disorders (oppositional defiant disorder, intermittent explosive disorder, conduct disorder, antisocial personality disorder, pyromania, kleptomania)
For each category, we assessed resource availability (extensive/moderate/limited/very limited), identified gaps, and analyzed cultural/technological adoption patterns.
This categorization is one possible one among many. The complexity and ontological uncertainty of mental health as a field (at least in terms of nosology and diagnosis) is reflected in the abundance of various frameworks, such as the National Institute of Mental Health's Research Domain Criteria, research by the Hierarchical Taxonomy of Psychopathology, the Diagnostic and Statistical Manual, and the Psychodynamic Diagnostic Manual and related frameworks.
Key Finding: Dramatic Workforce Disparities
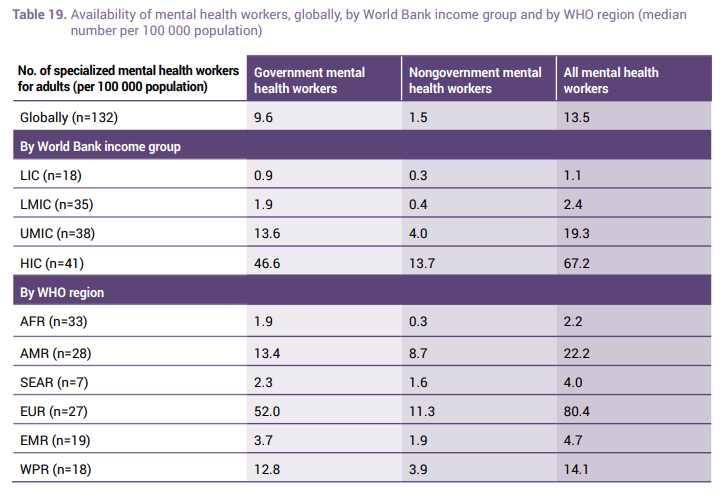
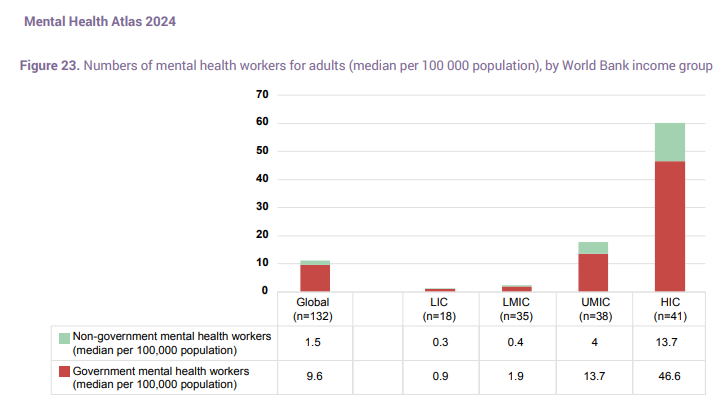
Using the latest WHO Mental Health Report data, we identified severe disparities in mental health workforce availability:
Global averages by World Bank income group (specialized mental health workers per 100,000 population):
- High-Income Countries (HIC): 67.2
- Upper-Middle-Income Countries (UMIC): 19.3
- Lower-Middle-Income Countries (LMIC): 2.4
- Low-Income Countries (LIC): 1.1
By WHO region:
- EUR (Europe): 80.4 per 100k
- AMR (Americas): 22.2 per 100k
- WPR (Western Pacific): 14.1 per 100k
- EMR (Eastern Mediterranean): 4.7 per 100k
- SEAR (South-East Asia): 4.0 per 100k
- AFR (Africa): 2.2 per 100k
This represents a 60-fold difference between highest and lowest resourced regions. In practical terms: a person with depression in Norway has access to ~80 mental health workers per 100,000 people, while someone in Uganda has access to ~0.1 – an 800-fold difference.
The Trauma-Tyranny Cycle: A Developmental Perspective on Long-Term Impact
Beyond immediate suffering, untreated mental health conditions – particularly trauma-related disorders and resulting attachment pathology – contribute to a self-perpetuating cycle that shapes political stability and conflict risk across generations.
The Cycle Model
The cycle operates as follows:
- Wars, societal collapse, and adverse childhood experiences → cause widespread trauma and chronic stress
- Trauma and parental mental health problems → disrupt healthy attachment formation in children
- Insecure attachment and unprocessed trauma → increase the susceptibility to (and rate of) power-seeking dictators
- Authoritarian leadership and poor institutional decision-making → increases risk of wars and societal collapse, perpetuating the cycle
This framework suggests that mental health interventions – particularly those addressing trauma, attachment, and personality pathology – have downstream effects on political stability, institutional quality, and conflict risk that compound across generations.
Evidence Base
Research supporting elements of this cycle:
- Trauma transmission: Parental trauma predicts insecure attachment in children; war trauma affects parenting practices across generations
- Attachment and leadership: Studies link insecure attachment patterns to authoritarian followership and preference for "strong man" leaders
- Personality pathology and power: Cluster B traits (particularly NPD and ASPD) overrepresented in positions of political power
- Developmental origins: Most personality disorders rooted in childhood trauma, neglect, and attachment disruption
- Malleability: Personality pathology treatable; attachment patterns can shift; trauma can heal – suggesting interventions can break the cycle
Why This Matters for Prioritization
This framework suggests we should weight conditions not only by immediate burden but by their role in perpetuating intergenerational cycles of suffering and instability:
High long-term impact conditions:
- PTSD and complex trauma: Direct cycle driver; prevents secure parenting
- Personality disorders (especially Cluster B): Direct link to power-seeking and authoritarian tendencies
- Attachment-disrupting conditions: Depression, anxiety, substance use in parents affect children's attachment security
- Childhood conduct problems: Early intervention prevents crystallization into ASPD
High-risk populations:
- Conflict-affected regions: Active cycle perpetuation; highest intervention value
- Parents and prospective parents: Breaking intergenerational transmission
- Adolescents and young adults: Critical window before personality patterns rigidify and before they become parents
Intervention modalities with cycle-breaking potential:
- Trauma healing: Reduces transmission to next generation
- Parenting support: Directly improves children's attachment security
- Personality disorder treatment: Reduces power-seeking behavior; improves parenting
- Resilience building: Strengthens population-level resistance to authoritarian messaging
This lens makes conditions like PTSD, personality disorders, and perinatal mental health higher priority despite some challenges, because successfully treating one generation protects the next.
Prioritization Framework
We developed a multi-tier framework weighing 20+ criteria across seven domains:
Tier 1: Core Feasibility
Safety & Risk Profile
- Can we deliver interventions without significant risk of harm?
- Do we have robust crisis protocols for high-risk situations?
- Can we reliably identify and escalate emergencies?
Key insight: This criterion should filter out conditions before other considerations. Active psychosis, acute suicidality, severe eating disorders in crisis, and mania present risks that outweigh potential benefits of unsupervised AI intervention.
Language Capacity
- Does our team have native/fluent speakers for seeking feedback, noticing and responding to problems?
- Can we avoid mere translation in favor of genuine cultural competence?
Technology Access & Literacy
- Smartphone penetration in target regions
- Data costs relative to local income
- Digital literacy rates
- Internet infrastructure reliability
Equity & Justice
- Prioritizing most underserved over most profitable
- Ensuring accessibility for lowest-income users
Cultural Sensitivity
- Avoiding imposition of Western psychiatric models on non-Western contexts
- Incorporating local healing traditions
- Collaborating with local communities and professionals
Transparency & Limitations
- Clear communication about AI capabilities and limitations
- Avoiding dependency creation
- Providing pathways to human care
Tier 2: Impact Potential
Mental Health Workforce Gap
- Where is the treatment gap largest?
- Where will AI provide the highest marginal benefit?
Disease Burden & Prevalence
- DALYs (Disability-Adjusted Life Years) lost
- Absolute number of people affected
- Regional variation in prevalence
Stigma & Barriers to Traditional Care
- Where does stigma prevent help-seeking?
- Where do cultural/gender restrictions limit access to human therapists?
- Where might anonymous AI access lower barriers?
Attachment Security Impact
- Does treating this condition improve parenting capacity?
- Will treatment reduce transmission of insecure attachment to children?
- Does the condition directly disrupt attachment formation?
High impact: Perinatal depression/anxiety, PTSD, substance use, personality disorders (all affect parenting)
Moderate impact: Depression, anxiety in parents; childhood trauma-related conditions
Power-Seeking & Authoritarianism Risk
- Does the condition involve patterns associated with malevolent leadership? (NPD, ASPD, sadism)
- Does healing reduce power-seeking behavior or improve use of power?
- Does treatment reduce susceptibility to authoritarian messaging?
High impact: Cluster B personality disorders, especially NPD/ASPD combinations; trauma creating "might makes right" worldviews
Moderate impact: Any condition improving emotional regulation and reducing reactivity to threats
Conflict & Instability Risk
- Is the condition prevalent in conflict zones, perpetuating cycles?
- Does the condition directly increase interpersonal violence risk?
- Does healing improve institutional decision-making quality?
High impact: PTSD in conflict zones, ASPD, substance use disorders, impulse control disorders
Moderate impact: Conditions affecting judgment and emotional regulation
Critical Developmental Windows
- Can we intervene before personality patterns rigidify? (adolescence/early adulthood)
- Can we intervene before individuals become parents?
- Can we heal parents before patterns transmit to children?
High impact: Adolescent/young adult populations; perinatal interventions; parenting support
Population-Level Resilience
- Does healing this condition make populations more resistant to manipulation?
- Does treatment promote secure attachment at scale?
- Does intervention build what Antonovsky calls "sense of coherence" (comprehensibility, manageability, meaningfulness)?
High impact: Trauma healing, attachment-focused interventions, mental health literacy programs
Tier 3: AI Suitability
Amenability to Structured Interventions
AI is most effective for conditions with structured, manualized treatments:
- Excellent fit: CBT for depression/anxiety, CBT-I for insomnia, exposure protocols, behavioral activation, psychoeducation
- Moderate fit: Motivational interviewing, DBT skills training, habit tracking, mentalization practice
- Poor fit: Complex trauma requiring relational depth, severe personality disorders needing nuanced therapeutic tensions, conditions requiring physical examination
Self-Help Amenability
- Does evidence support self-directed interventions?
- Can people improve without immediate professional involvement?
Data & Training Resources
- Quality of LLM training data for condition
- Availability of evidence-based treatment manuals
- Ability to validate AI responses against gold standards
Tier 4: Market Gap Analysis
Existing Digital Solutions
- Where are markets oversaturated vs. underserved?
- Where do existing solutions fail to serve LMICs?
Our finding: Dramatic inequality mirrors workforce gaps. Most mental health apps target English-speaking HIC markets. Very few quality apps exist in Hindi (500M+ speakers), Bengali (230M+ speakers), or Tamil (80M+ speakers). African markets almost entirely neglected except South Africa.
Cultural Adaptation Needs
- Where do Western psychiatric models fail to translate?
- Where is somatic expression of distress more common?
- Collectivist vs. individualist therapy frameworks
Existing Workbook/Professional Resource Availability
- Can we adapt existing evidence-based resources?
- Do gaps indicate lack of proven interventions or just lack of accessibility?
Tier 5: Strategic Considerations
Scalability Potential
- Size of potential user base
- Growth trajectory of condition awareness/diagnosis
- Platform effects and community features
Regulatory & Liability Landscape
- Regulatory requirements vary by region and intervention type
- Risk increases with diagnostic/treatment claims vs. psychoeducation/support
Monetization Potential
- Willingness to pay varies by region and condition
- Venture capital funding opportunities
- Grant funding opportunities (WHO, NGOs, government programs)
- Freemium viability for impact at scale
Partnership Opportunities
- NGO/WHO initiatives in target regions
- Research institutions for validation studies
- Local healthcare systems for integration
- Telehealth providers for triage/adjunct services
Measurement & Validation
- Can we measure impact using validated scales?
- Feasibility of clinical validation studies
- User engagement and retention metrics
Condition Prioritization: Rankings and Rationale
Using this framework, we ranked conditions by overall suitability. Note that the assessment of fuzzy regional factors of suitability is heavily informed by AI.
Tier 1: Highest Priority
PTSD (Prioritize Conflict-Affected Regions)
- Burden: High in conflict-affected regions (Afghanistan, Sudan, South Sudan, Syria, Yemen, DRC, Myanmar, Pakistan border regions, Northeast Nigeria)
- Gap: Extreme shortage of trauma-trained therapists
- AI Fit: Good – PE and CPT components are structured
- Safety: Moderate risk – requires robust crisis protocols
- Existing Resources: Very few culturally appropriate apps for conflict-affected LMICs
- Stigma: Extremely high in many cultures; AI may lower barriers
- Cultural: Trauma narratives culturally specific; requires careful adaptation
- Cycle Impact: ⭐⭐⭐⭐⭐ – PTSD is the primary cycle driver. Traumatized parents have difficulty providing secure attachment; PTSD directly transmits across generations via parenting practices and epigenetics; conflict-zone trauma creates conditions for the next generation of authoritarian leaders; healing trauma breaks the cycle at its source.
Personality Disorders – Strategic Focus on Cluster B (NPD, ASPD, BPD, HPD)
Our team's unique positioning: Given team lead's connections in NPD/ASPD/HPD communities and MBT training, we have potential advantages in serving this highly stigmatized population.
- Burden: ~10% of population; severe functional impairment
- Gap: MASSIVE stigma prevents help-seeking; very few specialists even in HICs
- AI Fit: MODERATE-DIFFICULT – MBT requires nuanced mentalizing that challenges AI, BUT psychoeducation and skill-building components could help
- Safety: Moderate-High risk depending on disorder (ASPD risk assessment, BPD self-harm)
- Existing Resources: Very limited for Cluster B; most resources focus on "surviving" people with NPD/BPD rather than helping them
- Cultural: Cluster B presentations culturally mediated; requires deep cultural knowledge
- Cycle Impact: ⭐⭐⭐⭐⭐ – This is the other primary cycle driver. Cluster B disorders (especially NPD and ASPD) are directly associated with power-seeking behavior, authoritarian leadership, and malevolent use of power. These conditions arise from childhood trauma and transmit intergenerationally through disrupted attachment. Healing personality disorders directly reduces the pool from which malevolent leaders emerge. BPD, while less associated with power-seeking, severely disrupts parenting and attachment.
The compassionate case: As I've argued elsewhere, people with NPD and ASPD are not “evil” – they are using brilliant childhood adaptations to survive impossible situations. These adaptations become maladaptive in adulthood but can heal with appropriate support, typically in just a few years of therapy. Many individuals with these conditions desperately want help but cannot access it due to stigma, cost, and scarcity of trained therapists.
The strategic case: The overlap between Cluster B traits and positions of power means that even small improvements in this population have outsized effects on institutional quality, conflict risk, and the next generation's wellbeing. If we can help even a fraction of people with these conditions, the downstream effects on politics, violence, and intergenerational trauma transmission could be substantial.
Possible approach: Focus on psychoeducation, mentalization skills practice, emotion regulation – NOT replacement for intensive therapy but potentially helpful adjunct for people unable/unwilling to access traditional care due to stigma. Clear about AI limitations. Strong safety protocols for violence risk. Initial target: adults with NPD/ASPD seeking help (not those court-mandated or uninterested in change).
Conduct Disorder / Childhood Trauma Interventions
- Burden: Common in high-adversity environments
- Gap: Very few child mental health services in LMICs
- AI Fit: Moderate – parenting interventions structured; child-facing interventions more challenging
- Safety: Moderate – requires careful age-appropriate design
- Challenges: Would need separate child-focused platform; consent/privacy issues
- Cycle Impact: ⭐⭐⭐⭐⭐ – Early intervention prevents personality disorder crystallization. Conduct disorder is precursor to ASPD; childhood trauma is the root cause of most personality pathology. Intervening in childhood/adolescence is the most effective cycle-breaking point, before patterns rigidify. Biggest challenge: reaching children requires a different platform approach.
Perinatal Mental Health (Depression, Anxiety)
- Burden: Massive need in your regions (maternal mortality links)
- Gap: Low resources for perinatal mental health
- AI Fit: Good for psychoeducation, CBT components
- Safety: Moderate-High risk (infanticide, severe postpartum psychosis require emergency response)
- Opportunity: WHO priority area; partnership potential
- Cycle Impact: ⭐⭐⭐⭐⭐ – This is a peak intervention point for attachment security. Perinatal mental health directly affects infant attachment formation; this is the most critical developmental window; treating mothers prevents transmission to the next generation at the source.
Tier 2: High Priority
Depression (Mild–Moderate)
- Burden: Leading cause of disability globally; ~280M people affected
- Safety: Low risk if severe/suicidal cases properly filtered and escalated
- AI Fit: Excellent – CBT and behavioral activation are highly structured
- Evidence: Strong self-help efficacy data
- Workforce Gap: Massive gap in LIC/LMIC (treatment gap >80%)
- Existing Resources: Many apps exist BUT dramatic language gap (almost nothing quality in Hindi/Tamil/Bengali for LMIC contexts)
- Measurement: PHQ-9 validated globally
- Cultural: Depression presents across cultures but may manifest somatically – requires adaptation
- Cycle Impact: ⭐⭐⭐ – Parental depression significantly disrupts attachment security; reduces parenting capacity; transmits intergenerationally
Anxiety Disorders (GAD, Social Anxiety, Panic)
- Burden: ~300M affected globally; highly disabling
- Safety: Low risk
- AI Fit: Excellent – CBT protocols, exposure hierarchies, grounding techniques all structured
- Evidence: Strong self-help efficacy
- Gap: Similar to depression – huge LMIC gap, language barriers
- Measurement: GAD-7, SPIN validated globally
- Cultural: Anxiety universal but expression varies; requires cultural adaptation
- Cycle Impact: ⭐⭐⭐ – Anxious parenting affects children's attachment security; hypervigilance transmits intergenerationally; anxiety increases susceptibility to threat-based authoritarian messaging
Substance Use Disorders (Harm Reduction Focus)
- Burden: Major cause of DALYs in many LMICs
- Gap: Extreme stigma prevents help-seeking; very few services
- AI Fit: Good for motivational interviewing, harm reduction education, tracking
- Safety: Moderate – requires crisis protocols for overdose risk, withdrawal
- Cultural: Highly stigmatized; AI anonymity major advantage
- Challenges: Cultural/religious sensitivities (alcohol in Muslim countries, substance use stigma in conservative societies)
- Cycle Impact: ⭐⭐⭐⭐ – Parental substance use severely disrupts attachment; increases violence and neglect; intergenerational transmission common; substance use associated with impulsive violence and poor institutional decision-making
Tier 3: Medium to Low Priority
Insomnia (Primary & Comorbid)
- Burden: ~30% of adults affected; impacts physical and mental health
- Safety: Zero acute risk
- AI Fit: PERFECT – CBT-I is highly manualized and structured
- Evidence: CBT-I self-help proven effective (comparable to therapist-delivered)
- Gap: Very few quality apps in target languages despite universal problem
- Measurement: Sleep diary, ISI scale
- Cultural: Low stigma = higher engagement; universal relevance
- Unique advantage: "Gateway" condition – treating insomnia often improves comorbid depression/anxiety
- Cycle Impact: ⭐⭐ – Better sleep improves emotional regulation and parenting quality; indirect effects on attachment security
OCD
- Burden: Highly disabling; ~2–3% prevalence
- AI Fit: Excellent – ERP is highly structured
- Gap: Very few ERP-trained therapists even in HICs
- Safety: Low risk, beyond the danger of reinforcing compulsions
- Existing Resources: Few quality apps in any language
- Cultural: Presentations vary (religious scrupulosity, contamination fears vary culturally)
- Cycle Impact: ⭐ – Minimal direct effect on attachment or power-seeking, though severe OCD can impair parenting
ADHD (Adults & Adolescents)
- Burden: Growing awareness in LMICs; severe underdiagnosis
- AI Fit: Excellent for skills training (time management, organization, emotional regulation)
- Safety: Zero acute risk
- Gap: Massive – most LMICs have near-zero ADHD services for adults
- Existing Resources: MANY productivity apps BUT few culturally adapted for India/Africa; mostly assume HIC work contexts
- Cultural: ADHD increasingly recognized cross-culturally but stigma varies
- Cycle Impact: ⭐⭐ – Untreated ADHD in parents complicates parenting; emotion dysregulation affects children; but not directly linked to power-seeking or authoritarianism
Somatic Symptom Disorders
- Burden: Very common in target regions (somatic expression of distress culturally normative in many Asian/African contexts)
- Gap: Almost NO existing digital resources
- Cultural Fit: Highly relevant – Western psychology often fails to address
- Challenges: Requires medical rule-outs (liability risk); validation complex
- Opportunity: Major gap to fill with culturally appropriate approaches
- Cycle Impact: ⭐⭐ – Chronic pain/illness affects parenting capacity; but not directly linked to attachment disruption or power-seeking
Bipolar Disorder
- High safety risk (mania, suicidality)
- Medication essential (beyond AI scope)
- Complex case management needs
- Cycle Impact: ⭐⭐ – Untreated bipolar disrupts parenting, but with medication most people stable
Eating Disorders
- High medical risk requiring monitoring
- Lower prevalence in initial target regions (though rising)
- Complex interventions
- Cycle Impact: ⭐ – Minimal direct cycle effects except in severe cases affecting parenting
Psychotic Disorders
- HIGH safety risk
- Medication usually essential
- Anosognosia limits engagement
- BUT: Family psychoeducation could be valuable supportive intervention
- Cycle Impact: ⭐ – Most people with schizophrenia are not violent or power-seeking; primary impact is on individual/family suffering
Geographic Prioritization: Country Rankings
Using mental health workforce data (per 100,000 population), World Bank income classifications, language accessibility, technology infrastructure, and conflict/trauma exposure, but ignoring strategic, marketing, or funding considerations. Fuzzy regional, cultural, and historical impressions again draw heavily on AI.
Tier 1: Highest Priority Markets 🎯
India
- Mental health workers: ~0.3–0.6 per 100k (vs. 67.2 in HICs)
- Population: 1.43 billion
- Languages: Hindi (550M speakers), Tamil (80M speakers), English (widespread)
- Income: LMIC (but wide internal variation)
- Technology: Rapidly growing smartphone penetration; good mobile infrastructure in urban/suburban areas
- Mental Health Burden: High rates of depression, anxiety, suicide
- Conflict/Trauma: Kashmir conflict; communal violence; high rates of adverse childhood experiences
- Cycle Status: ⭐⭐⭐ – Significant trauma exposure; growing but incomplete mental health infrastructure; critical window to intervene before patterns rigidify
- Rationale: Largest addressable market with our language capabilities; enormous gap; growing mental health awareness
- Challenges: Digital divide (rural vs. urban); data costs; diverse cultural contexts
Pakistan
- Mental health workers: ~0.2–0.5 per 100k
- Population: 231 million
- Languages: English (official), Urdu (mutually intelligible with Hindi)
- Income: LMIC
- Technology: Growing smartphone adoption; less infrastructure than India
- Mental Health Burden: High; extreme stigma particularly around women's mental health
- Conflict/Trauma: Afghan border terrorism; internal sectarian violence; TTP attacks; drone strike trauma; significant PTSD burden
- Cycle Status: ⭐⭐⭐⭐ – Active conflict perpetuating trauma cycles; very low mental health capacity; strong stigma preventing help-seeking
- Rationale: Second-largest Urdu/Hindi-speaking population; severe gap; AI anonymity crucial given stigma; trauma healing critical for conflict de-escalation
- Challenges: Political instability; conservative cultural norms; lower female digital access
Afghanistan
- Mental health workers: ~0.02–0.05 per 100k (among world's lowest)
- Population: 41 million
- Languages: English (limited), but potential Dari/Pashto development
- Income: LIC
- Technology: Growing mobile penetration despite infrastructure challenges
- Mental Health Burden: Extreme – decades of war
- Conflict/Trauma: 40+ years continuous conflict; Taliban rule trauma; highest trauma burden globally
- Cycle Status: ⭐⭐⭐⭐⭐ – Active cycle perpetuation at crisis levels. Entire generations traumatized; minimal mental health infrastructure; current authoritarianism driven by trauma cycles. Highest need but also highest access barriers.
- Rationale: Most acute trauma burden; greatest potential cycle-breaking impact
- Challenges: Security situation; female access restrictions; language barrier (would need Dari/Pashto); political complications
Nigeria
- Mental health workers: ~0.2–0.3 per 100k
- Population: 220 million
- Languages: English (official)
- Income: LMIC
- Technology: Variable – good in urban areas, limited in rural
- Mental Health Burden: High; stigma extreme
- Conflict/Trauma: Boko Haram in northeast (mass trauma, kidnappings); farmer-herder violence; Niger Delta conflict; significant PTSD burden
- Cycle Status: ⭐⭐⭐⭐ – Active conflict zones; trauma perpetuating instability; religious extremism linked to trauma cycles
- Rationale: Largest African market; English-speaking; enormous gap; trauma healing critical in conflict zones
- Challenges: Infrastructure variability; cultural diversity (250+ ethnic groups); data costs; religious considerations
South Sudan
- Mental health workers: <0.05 per 100k
- Population: 11 million
- Languages: English (official)
- Income: LIC
- Technology: Very limited but growing mobile access
- Mental Health Burden: Extreme – ongoing conflict
- Conflict/Trauma: Continuous war since independence; mass displacement; extreme violence exposure; one of world's highest trauma burdens
- Cycle Status: ⭐⭐⭐⭐⭐ – Acute cycle perpetuation; virtually no mental health services; urgent intervention needed
- Rationale: Desperate need; English-speaking; potential for enormous impact
- Challenges: Infrastructure extremely limited; ongoing conflict; very low literacy
Democratic Republic of Congo
- Mental health workers: ~0.05 per 100k
- Population: 99 million
- Languages: French (official), some English
- Income: LIC
- Technology: Growing mobile penetration despite poor infrastructure
- Mental Health Burden: Extreme – decades of conflict
- Conflict/Trauma: 25+ years of war; mass rape as weapon; child soldiers; extreme violence; ongoing Eastern Congo conflict
- Cycle Status: ⭐⭐⭐⭐⭐ – Severe trauma perpetuating instability; virtually no services
- Rationale: Massive trauma burden; enormous need
- Challenges: Language barrier (would need French); infrastructure; ongoing violence; complexity
Myanmar
- Mental health workers: ~0.1 per 100k
- Population: 54 million
- Languages: English (some), Mandarin (some)
- Income: LMIC
- Technology: Previously growing, now complicated by military coup
- Mental Health Burden: High and worsening
- Conflict/Trauma: Military coup trauma; Rohingya genocide; ethnic conflicts; civil war
- Cycle Status: ⭐⭐⭐⭐⭐ – Active authoritarian violence; trauma-driven conflict cycles; dramatic example of cycle in action
- Rationale: Clear case of trauma-tyranny cycle; potential intervention point
- Challenges: Political situation; military restrictions; language barriers; safety concerns
Kenya
- Mental health workers: ~0.5 per 100k
- Population: 54 million
- Languages: English, Swahili
- Income: LMIC
- Technology: Relatively advanced mobile infrastructure (M-Pesa model)
- Mental Health Burden: Moderate rates; growing awareness
- Conflict/Trauma: Post-election violence (2007–08); Al-Shabaab attacks; inter-ethnic tensions
- Cycle Status: ⭐⭐⭐ – Historical trauma; relatively stable now but at risk; preventive intervention valuable
- Rationale: Best African tech infrastructure; English-speaking; relatively strong civil society; good test case for preventive approach
- Challenges: Would need Swahili for broader reach
Bangladesh
- Mental health workers: ~0.1–0.2 per 100k
- Population: 170 million
- Languages: Bengali/English
- Income: LMIC
- Technology: Rapidly improving mobile infrastructure
- Mental Health Burden: High rates of depression, anxiety
- Conflict/Trauma: Liberation war trauma (1971); Rohingya refugee crisis; natural disasters; high rates of interpersonal violence
- Cycle Status: ⭐⭐⭐ – Historical trauma; refugee crisis stress; refugee population particularly high-need
- Rationale: Large Bengali-speaking population; severe gap; growing digital access; Rohingya camps could be specific intervention target
- Challenges: Would require Bengali language development (related to Hindi but distinct)
Yemen
- Mental health workers: ~0.02–0.05 per 100k
- Population: 33 million
- Languages: Arabic (no team capacity currently)
- Income: LIC
- Technology: Infrastructure severely damaged by war
- Mental Health Burden: Extreme – humanitarian catastrophe
- Conflict/Trauma: Ongoing civil war; Saudi bombing; famine; cholera; complete societal breakdown
- Cycle Status: ⭐⭐⭐⭐⭐ – Worst humanitarian crisis globally; entire population traumatized; desperately needs intervention
- Rationale: Extreme need; enormous potential impact if accessible
- Challenges: Language barrier (would need Arabic); infrastructure destroyed; ongoing war; access extremely limited
Tier 2: Secondary Priority Markets
Syria (ongoing conflict, Arabic language barrier but extreme need)
Ethiopia (123M, recent Tigray conflict, English educational language)
Sudan (46M, ongoing conflict, English secondary)
Tanzania (65M, LIC, English/Swahili)
Uganda (47M, LIC, English, LRA conflict legacy)
Nepal (30M, LMIC, English, Hindi understood, Maoist conflict legacy)
Open Questions and Request for Feedback
We welcome any feedback, and are particularly interested in:
- Prioritization blind spots. What important criteria are we missing? What are we overweighting or underweighting?
- Funding and partnerships. Can we safely bootstrap in the US with VC funding and expand to other countries later?