Global Health Landscape
By DavidNash @ 2025-07-21T11:28 (+30)
I thought it would be useful to have a more up to date overview of the field, especially the funding side.
Often in the news you'll hear of millions or billions being spent or cut from different government programs or healthcare interventions, but with no context on whether that is a relatively large or small amount, and how much we should calibrate our concern/completely shift our focus.
Without some understanding the ~$10 trillion global health system, it's difficult to evaluate these announcements properly or identify where efforts might have more impact.
This is the second part of week 2 of my series on global development.
The Current Global Health Landscape
Global health is a field focused on improving health for all people worldwide, often with particular focus on improving health outcomes for the world's poorest and most vulnerable populations. There can be challenges that transcend national boundaries and require collective/international action but it also covers countries improving their own health systems.
Understanding the global distribution of disease and mortality offers useful context for seeing how everything fits together.
- Our World in Data - An overview of our research on global health (10 minutes)
Several key trends:
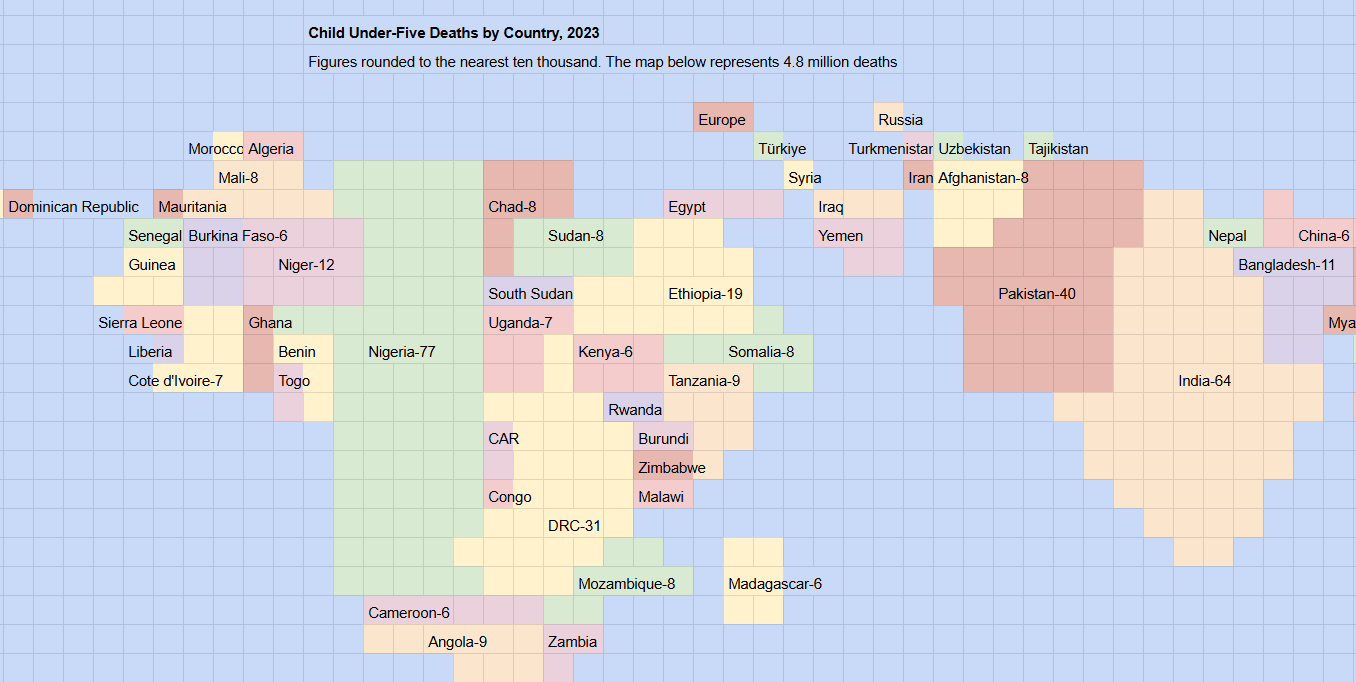
Declining mortality rates: Child mortality rates have decreased significantly worldwide but remain much higher in low-income countries
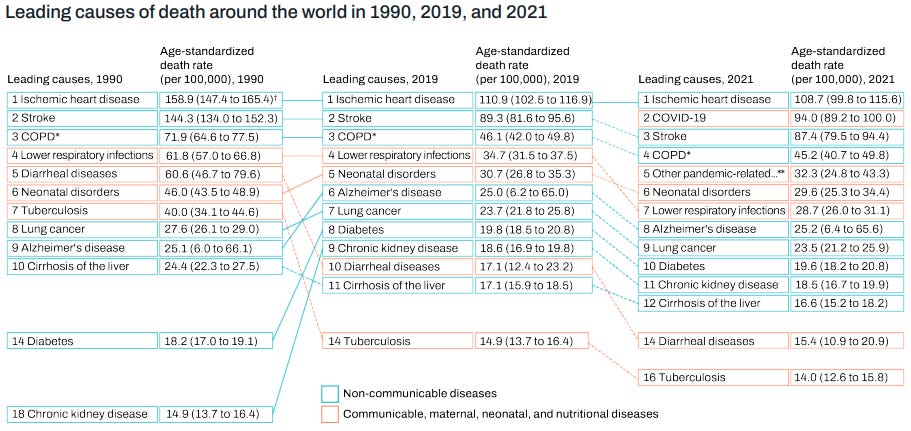
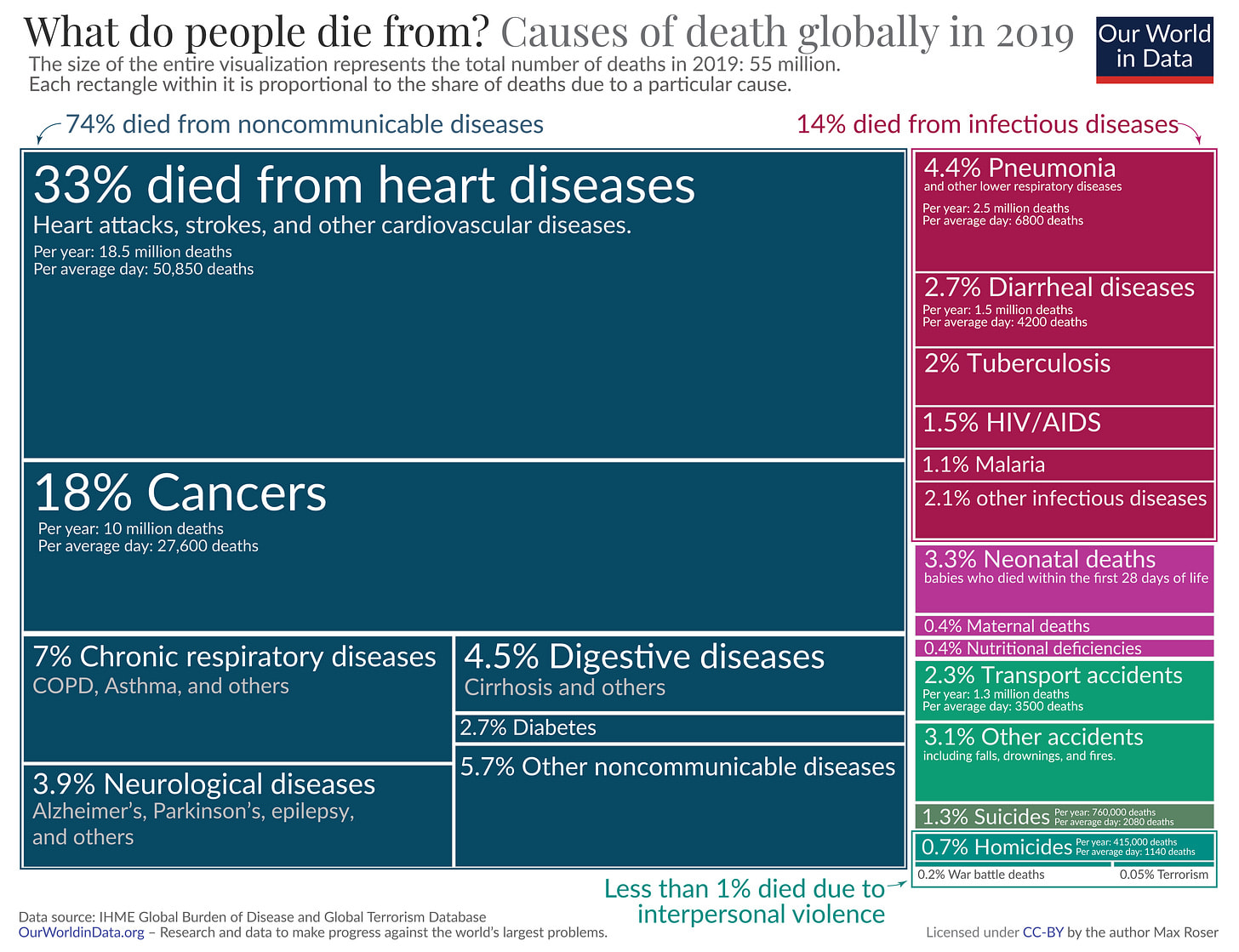
- Shifting disease burden: Non-communicable diseases like heart disease and diabetes now account for approximately 74% of global deaths
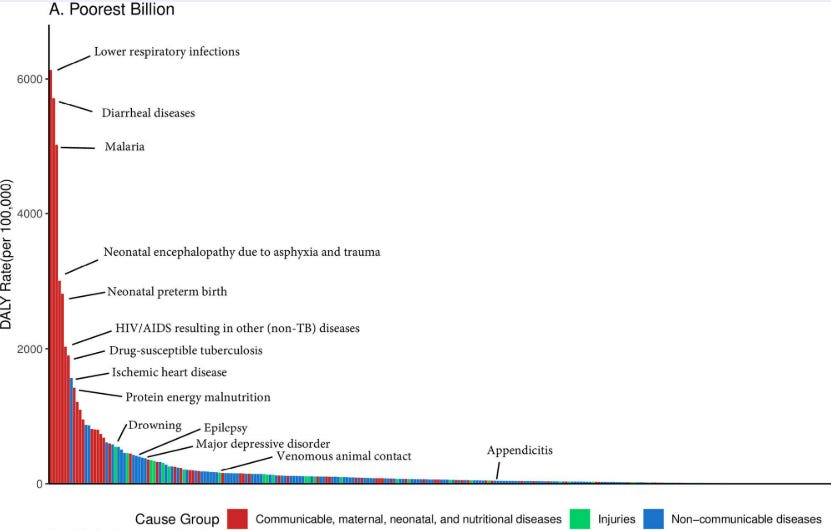
- Persistent issues: Health challenges disproportionately affect certain regions and populations, with the poorest billion people bearing a much higher burden of preventable disease
Global Mortality Trends
The leading causes of death worldwide have evolved significantly between 1990 and 2021. While communicable diseases remain prominent in low-income settings, non-communicable diseases now dominate global mortality statistics. More recently, the COVID-19 pandemic has further altered this landscape.
Health Outcome Disparities
Despite progress, the burden of disease is not evenly distributed:
- Communicable diseases continue to disproportionately affect the poorest populations
- Life expectancy in low-income countries remains significantly lower than in high-income countries
- Within countries, the poorest and most vulnerable often face the greatest health challenges
Key Global Health Areas
Global health efforts are typically organised into areas addressing specific categories of disease and their influencing factors. The following represent major domains in contemporary global health practice:
- Non-communicable Diseases
- NCDs, including cardiovascular disease, diabetes, cancer and chronic respiratory conditions, now account for the majority of global deaths (around 74% in 2019)
- Their prevalence is rapidly increasing in lower-middle income countries (LMICs) where healthcare systems are often less equipped to manage chronic conditions
- Infectious Diseases/Communicable Disease
- Major persistent epidemics (HIV/AIDS, malaria, tuberculosis)
- Emerging threats (Ebola, COVID-19, "Disease X")
- Antimicrobial resistance
- Neglected tropical diseases affecting billions worldwide cumulatively
- Water, Sanitation, and Hygiene (WASH)
- Approximately 2 billion people globally lack access to safely managed drinking water, while 3.6 billion lack adequate sanitation. These deficiencies contribute to diarrhoeal diseases that:
- Cause ~830,000 deaths annually
- Remain the second leading cause of death in children under five years
- Approximately 2 billion people globally lack access to safely managed drinking water, while 3.6 billion lack adequate sanitation. These deficiencies contribute to diarrhoeal diseases that:
- Maternal, Newborn, and Child Health (MNCH)
- This area addresses pregnancy-related health needs, childhood illnesses and nutrition affecting ~130 million births annually worldwide. Despite improvements, each year:
- Approximately 295,000 women die during pregnancy and childbirth
- Around 5 million children die under the age of 5
- This area addresses pregnancy-related health needs, childhood illnesses and nutrition affecting ~130 million births annually worldwide. Despite improvements, each year:
- Nutrition and Food Security
- Global nutrition challenges present in multiple forms:
- Approximately 828 million people faced hunger in 2021
- An estimated 149 million children under five suffer from stunting and 45 million from wasting
- Over 2 billion adults are overweight or obese, highlighting the "double burden" of malnutrition globally
- Global nutrition challenges present in multiple forms:
- Mental Health and Substance Use
- Mental health represents a growing global health priority:
- In 2019, an estimated 970 million people worldwide were living with a mental disorder, with depression and anxiety as the top two diagnosed conditions
- Mental health conditions account for approximately 14% of the global burden of disease
- Suicide claims nearly 800,000 lives annually
- Significant challenges persist in accurate diagnosis, with large variation between countries
- Mental health represents a growing global health priority:
- Health Systems
Health systems comprise the infrastructure, workforce, financing, innovation and governance that underpin health interventions. Systems worldwide vary greatly in their structures. Most health systems include:
- Primary healthcare and public health measures: The foundation of most effective health systems
- Varying governance structures: Some systems are decentralised with multiple stakeholders, while others are centrally coordinated
- Multiple actors: Including government entities, private providers, charitable foundations, religious institutions and professional medical associations
The strength and design of health systems significantly impact a country's ability to deliver effective interventions and respond to health challenges
- Environmental Health
- Environmental factors significantly impact global health:
- Air pollution is associated with approximately 7 million premature deaths annually
- Over 90% of the world's population breathes air that exceeds WHO guideline limits
- Chemical exposures, unsafe water, and climate change impacts contribute significantly to global disease burden
- Lead pollution contributes to 1% of the global disease burden
- Environmental factors significantly impact global health:
- Injury Prevention and Trauma Care
- Injuries represent a substantial but often overlooked health challenge:
- 4.4 million lives were lost due to injury in 2019 (8% of all deaths)
- Road traffic accidents (1.3 million deaths), violence, falls and burns result in millions of fatalities and injuries annually
- Injuries are the leading cause of death for people aged 5-29 years worldwide
- 93% of fatal road traffic injuries occur in LMICs
- Injuries represent a substantial but often overlooked health challenge:
- Sexual and Reproductive Health
- This domain encompasses family planning, STI prevention/treatment and sexual health services:
- Approximately 218 million women have an unmet need for modern contraception
- Over 38 million people live with HIV globally
- An estimated 357 million new cases of four curable STIs occur annually
- This domain encompasses family planning, STI prevention/treatment and sexual health services:
There are many more areas, sub-fields and cross-cutting topics related to global health, but the above are some of the main fields. They highlight the wide range of challenges and possible interventions.
Global Health Spending
Understanding how health systems are financed is fundamental to addressing global health challenges. The allocation of financial resources for health, directly impacts who can access healthcare, which services are available and the health outcomes of populations.
Knowledge of global health financing context can help us make more informed decisions when choosing careers, directing donations or advocating for policy changes.
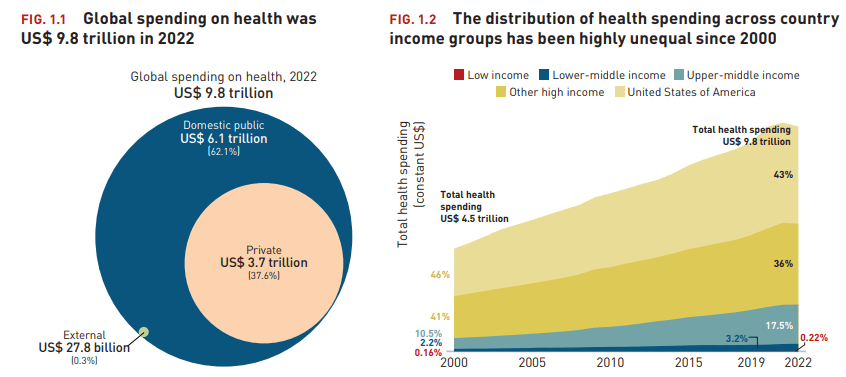
Total global spending on health reached $9.8 trillion in 2022 (about 10% of global GDP), more than doubling from $4.5 trillion in 2000. Health spending is made up of government expenditure, out-of-pocket payments (people paying for their own care), and sources such as voluntary health insurance, employer-provided health programs and activities by NGOs.
- High-income countries account for 79% of health spending (US alone is 43%)
- Domestic public spending accounts for 62%, while private spending represents 37.6% ($3.7 trillion)
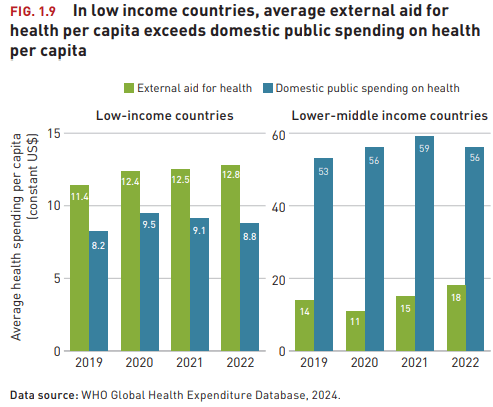
- External aid constitutes 0.3% ($27.8 billion) of global health expenditure, although this can be a larger proportion of spending in the poorest countries
- Our World in Data - Healthcare Spending (10 minutes)
- A comprehensive overview of global healthcare financing trends
Relationship Between Spending and Health Outcomes
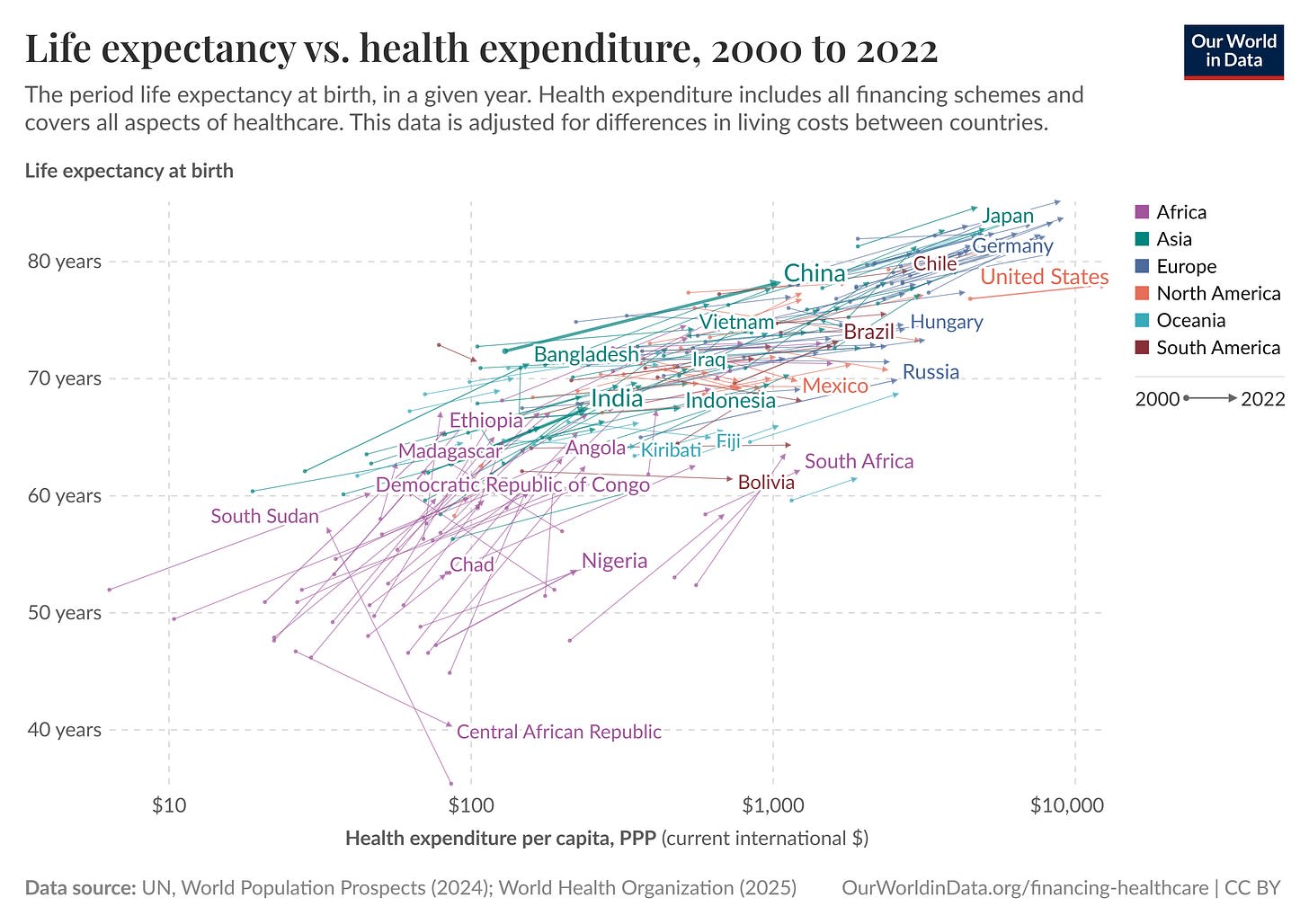
Healthcare spending per capita shows a positive correlation with life expectancy, though with diminishing returns as spending increases. This relationship is particularly evident when comparing countries across income groups:
- Low-income countries typically see significant gains in life expectancy with relatively modest increases in healthcare spending ($43 per capita)
- Middle-income countries experience continued improvements but at a decreasing rate per additional dollar spent ($132-$540 per capita)
- High-income countries show minimal marginal improvements despite substantially higher spending ($3,731 per capita)
This pattern suggests that initial investments in healthcare systems yield the greatest returns, particularly for basic interventions like vaccinations, maternal care and infectious disease control.
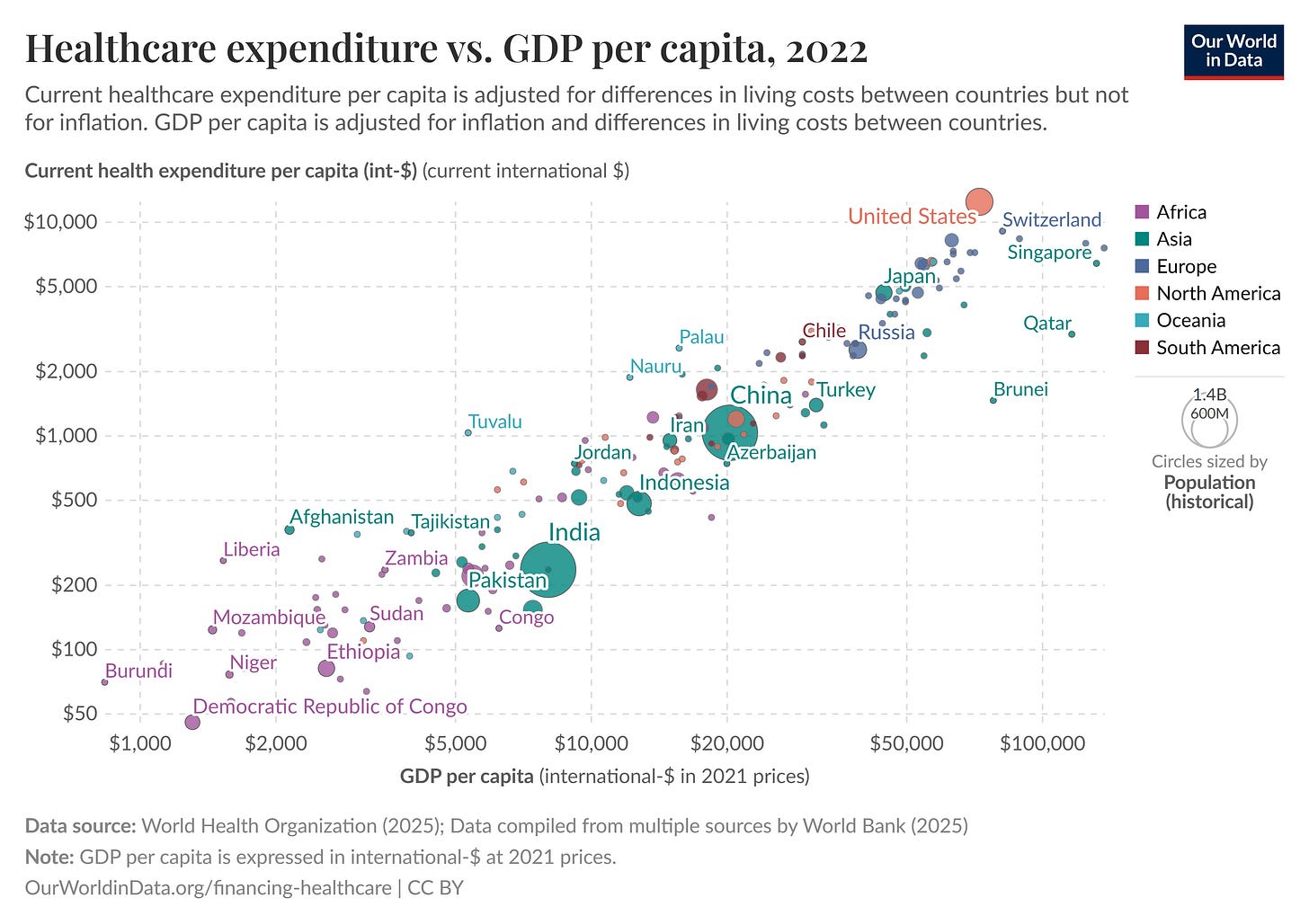
National Income and Health Investment
National income remains the strongest predictor of healthcare spending. This relationship is causal rather than merely correlational, as countries become wealthier, they allocate more resources to health through both public and private channels.
Sources of Healthcare Funding
Domestic vs External Funding
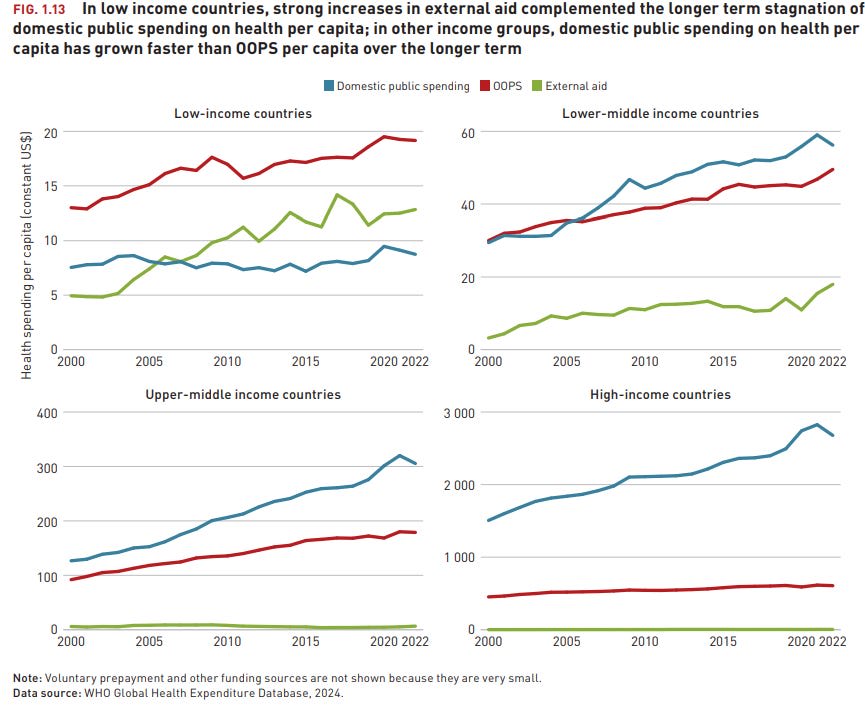
Healthcare systems are primarily funded through domestic sources (government and private sector (out of pocket spending)). However, the dependency on external donor funding varies significantly by economic development. This creates particular vulnerability for low-income countries, whose health systems may experience disruption when donor priorities shift.
Development Assistance
Since the establishment of the Millennium Development Goals in 2000, development assistance for health has increased significantly, especially for targeted areas like child mortality, maternal health, malaria and tuberculosis
Between 2000 and 2019, the share of health spending channelled through government schemes (mainly health budgets) and compulsory health insurance (mainly social health insurance) increased steadily except in low-income countries where it remained mostly unchanged.
- In the poorest countries (GDP per capita below $500), donor funding constitutes ~45% of health expenditure
- As countries develop economically, this external reliance steadily declines: to 34% for those with GDP per capita up to $1000
- Below 25% for nations up to $3000
Once countries exceed $3000 GDP per capita, external health funding typically represents less than 5% of total health expenditure
Health Financing Mechanisms
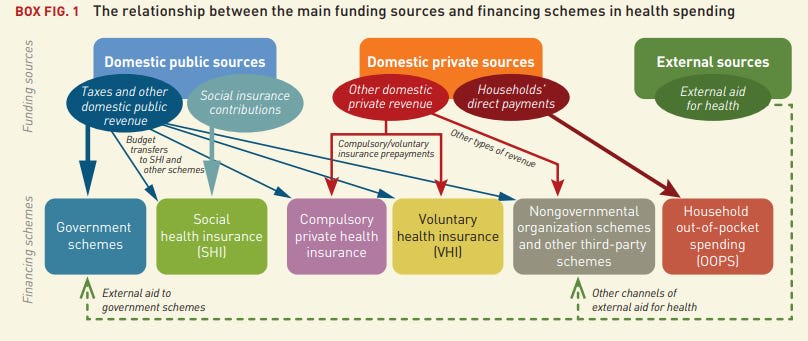
Healthcare financing comes through several key sources including public, private, out-of-pocket spending (OOPS) and external aid.
- Public Financing
- Government financing through general taxation or specific health taxes is the main funding for most healthcare systems. Countries with higher tax-to-GDP ratios generally achieve better health coverage with lower out-of-pocket expenses
- Health Insurance
- Health insurance mechanisms spread financial risk across populations, but differ in how they're funded, who's covered and who manages them.
- Government expenditure (tax-funded systems): Funded through general taxation, covers all citizens regardless of contribution, and is directly managed by government. Examples include the UK's NHS and Canada's Medicare
- Social Health Insurance (SHI): Typically mandatory, funded through dedicated payroll contributions (not general taxes), managed by quasi-public agencies or funds and traditionally linked to employment status. Examples include Germany's sickness funds and Japan's system. The number of countries with SHI schemes has risen significantly, particularly among middle-income countries
- Private Health Insurance (PHI): Private health insurance exists in most countries but varies greatly in its role and market share.
- Supplementary: Covers services beyond public provision (France, Canada, Australia)
- Duplicate: Offers faster access or provider choice alongside public systems (UK, Spain, Australia)
- Primary: Serves as main coverage for certain populations, sometimes being mandatory for all citizens (US, Switzerland, Netherlands)
- Health insurance mechanisms spread financial risk across populations, but differ in how they're funded, who's covered and who manages them.
- Out-of-Pocket Expenditure
- Direct payment at the point of service remains a significant financing mechanism in many low and middle-income countries. High out-of-pocket spending is associated with:
- Catastrophic health expenditure (defined as spending >10% of household income on health)
- Delayed or foregone care
- The WHO estimates that approximately 930 million people globally spend at least 10% of their household budget on healthcare.
- While the number of countries with out-of-pocket spending (OOPS) as the main health financing mechanism has declined since 2000, it remained the main financing scheme in 30 low and LMICs as of 2022. In 20 of these countries, OOPS accounted for more than half of total health spending.
- Direct payment at the point of service remains a significant financing mechanism in many low and middle-income countries. High out-of-pocket spending is associated with:
Innovative Financing
As traditional funding sources face constraints, new financing mechanisms are increasingly being suggested.
- Sin taxes on tobacco, alcohol and sugar-sweetened beverages, which both generate revenue and reduce consumption of harmful products
- Impact bonds that link investor returns to measurable health outcomes
- Blended finance mechanisms combining public, philanthropic and private capital
- Debt swaps for health, where external debt is forgiven in exchange for domestic health investments
The Future of Healthcare Financing
- Ageing populations globally will drive increased healthcare costs for non-communicable diseases and changing dependency ratios affecting social insurance mechanisms
- New health technologies present potential cost savings through telemedicine and digital health but also increased pressure to finance more expensive newer treatments and diagnostics
- New technologies in general could lead to faster economic growth, safer workplaces, cleaner energy, safer roads, etc leading to lower health demands
- Changing climates could impact temperature related deaths, crop success and migration, impacting health systems
- Changes in foreign aid could impact what does and doesn’t get funded in lower income countries and lead to shifting prioritisation by governments
You can see the rest of week 2 here, which includes career ideas and further resources.
Ulf Graf 🔹 @ 2025-07-21T18:20 (+7)
Thank you for a really good overview! I will use some of these numbers for my lectures about global health! I have not held lectures about global health for a couple of years so even if I have talked about most of these areas the numbers need to be updated. You covered it really well! :)
Kind regards,
Ulf Graf
SummaryBot @ 2025-07-21T16:09 (+1)
Executive summary: This comprehensive overview of the global health landscape—part of a broader series on global development—highlights the dramatic shifts in disease burden, persistent health disparities, and the crucial role of financing, arguing that understanding these patterns is essential for assessing health policy decisions, guiding career choices, and making informed philanthropic or advocacy efforts.
Key points:
- Global disease trends have shifted: While child mortality has declined, non-communicable diseases now account for 74% of global deaths, and disparities in health outcomes remain stark between and within countries.
- Global health includes a wide range of domains: Key focus areas span from infectious and non-communicable diseases to WASH, nutrition, injury prevention, maternal health, mental health, and environmental factors like air pollution.
- Health financing is heavily unequal: High-income countries account for 79% of global health spending, while low-income countries often rely on external aid, which can be volatile and insufficient.
- Initial healthcare investments have the highest returns: Spending in low-income countries yields significant life expectancy gains, supporting the importance of funding basic interventions like vaccination and maternal care.
- Health systems differ widely in design and effectiveness: Public systems, social health insurance, and out-of-pocket models each have distinct implications for access, equity, and outcomes.
- Future challenges and innovations loom: Demographic shifts, climate change, and new technologies will affect health burdens and financing strategies, necessitating adaptive, sustainable solutions.
This comment was auto-generated by the EA Forum Team. Feel free to point out issues with this summary by replying to the comment, and contact us if you have feedback.